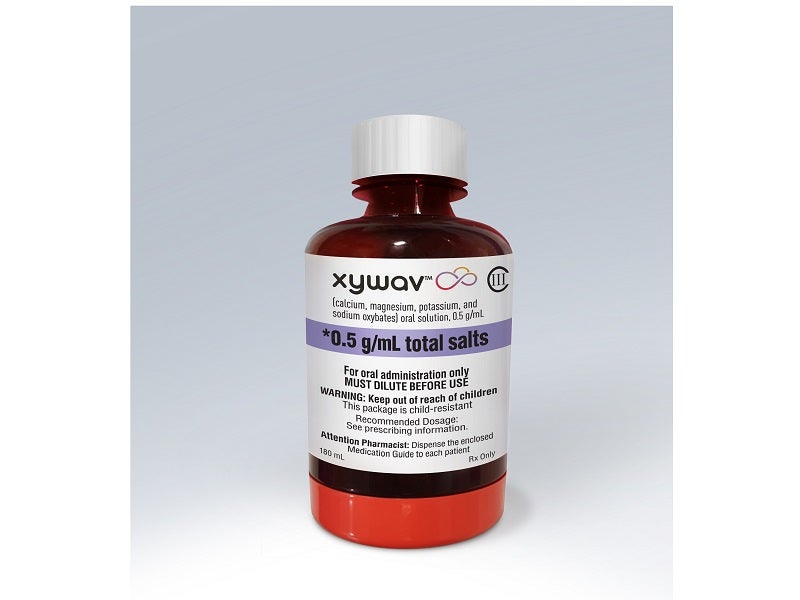
Jazz Pharmaceuticals’ XYWAV™ (calcium, magnesium, potassium, and sodium oxybates) is the first US Food and Drug Administration (FDA) approved medicine indicated for the treatment of cataplexy and excessive daytime sleepiness (EDS) associated with narcolepsy in over 15 years.
It contains 92% less sodium than Xyrem® (sodium oxybate), the current standard treatment recommended by the American Academy of Sleep Medicine (AASM) for patients with cataplexy and EDS.
XYWAV approvals
Jazz Pharmaceuticals submitted the new drug application (NDA) to the FDA for the approval of its JZP-258 oxybate investigational medicine in January 2020. The drug was accepted for priority review in March 2020.
The FDA approved XYWAV for the treatment of cataplexy or EDS in narcolepsy patients of age seven years and above in July 2020.
XYWAV (calcium, magnesium, potassium, and sodium oxybates) is available as an oral solution with a recommended initial dosage of 4.5g per night.
The drug should be introduced by the end of 2020 following the implementation of the risk evaluation and mitigation strategy (REMS).
To counter the risk of central nervous system (CNS) depression and abuse and misuse, it will be made available only through a restricted distribution programme known as Xywav and Xyrem REMS.
Cataplexy and narcolepsy causes and symptoms
Narcolepsy is a chronic, debilitating neurological disorder associated with an elevated risk of several comorbid disorders such as hypertension and cardiovascular diseases. Patients with the condition mainly suffer from EDS and uncontrollable sleep-wake cycles.
It is characterised by five main symptoms including cataplexy, EDS, disturbed overnight sleep, hypnagogic / hypnopompic hallucinations and sleep paralysis.
EDS is defined as a condition that involves the inability to stay awake or alert throughout the day, leading unintended lapses of drowsiness or sleep.
Cataplexy, considered the most specific symptom of narcolepsy, is an abrupt, brief loss of muscle tone with maintained consciousness and is activated by strong emotions.
XYWAV mechanism of action
The labelling of XYWAV carries a warning, which states that the drug is a CNS depressant. The medicine’s exact mechanism of action in treating narcolepsy is unclear.
XYWAV is a combination of calcium, magnesium, potassium, and sodium oxybate (gamma-hydroxybutyrate).
Gamma-hydroxybutyrate (GHB) is an endogenous substance that exists as a metabolite of the GABA neurotransmitter.
It is assumed that therapeutic effects of the drug on cataplexy and EDS are induced in noradrenergic and dopaminergic neurons, as well as thalamocortical neurons, through GABAB actions during sleep.
XYWAV has been classified as a Schedule III drug by the US Drug Enforcement Agency (DEA). Drugs, products, or chemicals with low to moderate potential for physical and psychological dependence fall under Schedule III category.
It is an oxybate drug made of cations that lead to 92% less sodium, equivalent to approximately 1,000 to 1,500mg a night than Xyrem® at a recommended 6-9g dose range.
Clinical trials on XYWAV
FDA approval is based on a global Phase III placebo-controlled, double-blind, randomised-withdrawal, multi-centre study that demonstrated the safety and efficacy of XYWAV for treating cataplexy and EDS in adult patients diagnosed with narcolepsy.
The study was conducted in two stages, of which the first stage involved the main study, while the second was an optional open-label extension (OLE) lasting 24 weeks.
The primary study had three phases, including an open-label optimised treatment and titration (OL OTTP) for 12 weeks, followed by a two-week stable dosage period and a double-blind randomised withdrawal period (DB RWP) for another two weeks.
A total of 201 patients, in the age group of 18 to 70 years, participated in the study. The medication showed significant differences in the number of cataplexy attacks per week and Epworth Sleepiness Scale (ESS) scores in comparison with placebo.
In the two-week DB RWP, 134 patients were randomised 1:1 to continue treatment with XYWAV or to placebo.
In 90% (62 / 69) of patients, the cumulative nightly dosage of XYWAV was given in two equal doses, while the remaining 10% (7 / 69) of patients were administered with unequal doses.
The primary outcome measure was the change in the weekly number of cataplexy attacks from the two weeks of open-label SDP to the two weeks of DB RWP, while the secondary endpoint was the change in the ESS Score from the end of the SDP to the end of the DB RWP.
The study also showed that the patients who stopped XYWAV therapy and were randomised to placebo during DB RWP experienced an increase in the average weekly number of cataplexy attacks and in the ESS score when compared to the participants randomised to continue JZP-258 treatment.
Common adverse reactions associated with JZP-258 during the study were nausea, anxiety, vomiting, parasomnia (a sleep disorder), excessive sweating (hyperhidrosis), diarrhoea, headache, decreased appetite and dizziness.