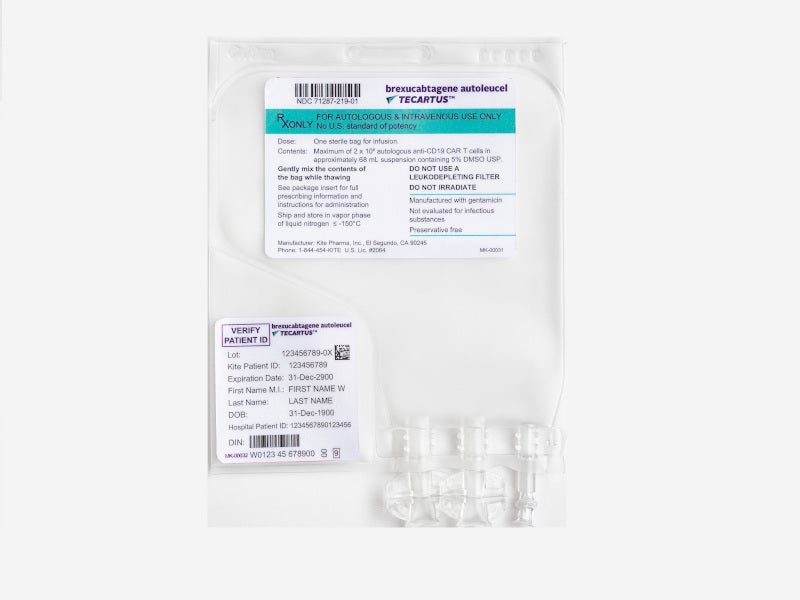
Tecartus™ (brexucabtagene autoleucel, formerly KTE-X19) chimeric antigen receptor (CAR) T-cell therapy is the first and only approved cell-based gene therapy for the treatment of mantle cell lymphoma (MCL).
Developed by Kite, a Gilead Company, Tecartus (brexucabtagene autoleucel) is a CD19-directed genetically modified autologous T-cell immunotherapy indicated for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (r / r MCL).
Tecartus (brexucabtagene autoleucel) is available as cell suspension for intravenous infusion. Each dose contains two 106 CAR-positive viable T-cells per kg of body weight, with a maximum of two 108 CAR-positive viable T-cells in approximately 68ml dispersion within an infusion bag.
Tecartus approvals
The biologics license application (BLA) for Tecartus (brexucabtagene autoleucel) was submitted to the US Food and Drug Administration (FDA) in December 2019 and accepted for review in February 2020.
The FDA granted accelerated approval to Tecartus (brexucabtagene autoleucel) for the treatment of adult patients with relapsed or refractory MCL in July 2020.
Tecartus was granted breakthrough therapy designation (BTD), priority review, and orphan drug designation by the FDA for the treatment of patients with relapsed or refractory MCL.
Tecartus received priority medicines (PRIME) status for r / r MCL by the European Medicines Agency (EMA), which is currently under assessment in the European Union (EU).
The FDA approved a risk evaluation and mitigation strategy (REMS) for Tecartus, which was paired with the Yescarta® (axicabtagene ciloleucel) REMS. It is currently known as the “Yescarta (axicabtagene ciloleucel) and Tecartus (brexucabtagene autoleucel) REMS Program”.
The FDA set a Prescription Drug User Fee Act (PDUFA) target action date of 10 August 2020.
Mantle Cell Lymphoma (MCL) causes and symptoms
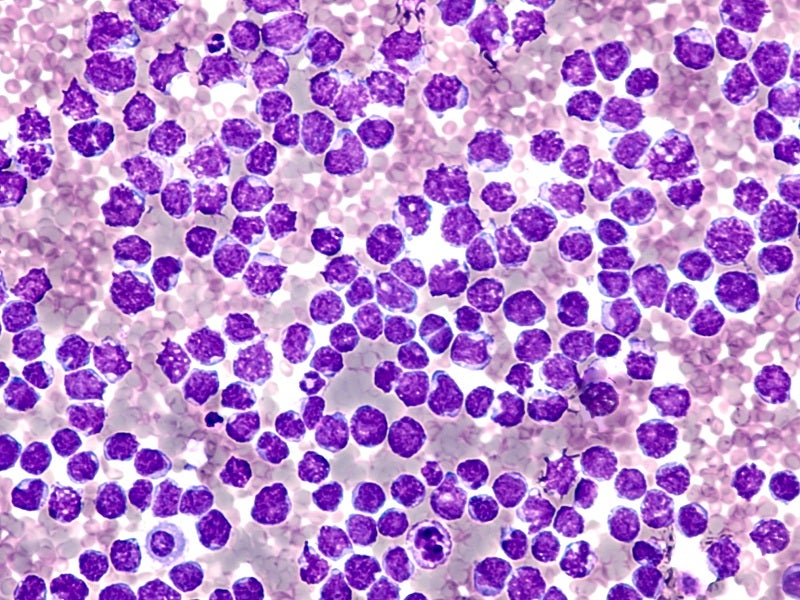
MCL is a rare type of cancerous B-cell non-Hodgkin lymphoma that typically develops from cells that reside in the lymph nodes mantle region and primarily affect middle-aged or older adults.
In MCL patients, B-cells, a white blood cell type that helps the body combat infection, turns into cancer cells, resulting in tumours in the lymph nodes. The cancer cells rapidly expand to other parts of the body.
MCL is considered incurable and most of the patients experience frequent relapse after initial treatment; its cause is mostly unknown.
Common symptoms of MCL include painless swelling in the armpit, neck or groin region, unexplained weight loss, night sweats, fever with no obvious cause, anaemia, diarrhoea, loss of appetite, sickness (nausea) and easy bruising or bleeding.
Tecartus mechanism of action
Tecartus is a genetically modified CD19-driven autologous T-cell immunotherapy that binds to cancer cells expressing CD-19, and normal B-cells.
It uses the manufacturing process XLP™ which involves T-cell enrichment, which is a critical step in some B-cell malignancies where circulating lymphoblasts is a common characteristic.
Studies have shown that the co-stimulatory domains CD28 and CD3-zeta trigger downstream signalling cascades that contribute to T-cell activation, proliferation, acquisition of effector functions, and secretion of inflammatory cytokines and chemokines following anti-CD19 CAR T-cell interaction with CD19-expressing target cells. This sequence of events contributes to the killing of cells that express CD19.
Tecartus is also currently undergoing phase I / II trials of acute lymphoblastic leukaemia (ALL) and chronic lymphocytic leukaemia (CLL), in addition to MCL.
Clinical trials on Tecartus
FDA approval of Tecartus is based on phase 2, open-label, single-arm and multicentre ZUMA-2 pivotal clinical trial.
The study enrolled 74 patients with relapsed or refractory MCL previously treated with anthracycline or bendamustine-containing chemotherapy, an anti-CD20 antibody, and a Bruton tyrosine kinase inhibitors (BTKi) ibrutinib or acalabrutinib.
All the enrolled patients underwent leukapheresis; five patients did not receive conditioning chemotherapy or Tecartus, while three endured production failure and one died from chronic disease and one patient withdrew from the trial.
One patient received lymphodepleting chemotherapy, but Tecartus was not administered due to continued persistent atrial fibrillation.
In the study, 60 patients were followed up for at least six months following their first reliable response to the disease, marking them as efficacy-evaluable.
Among the 60 patients evaluable for efficacy, 54 patients were administered two 106 CAR-positive viable T-cells per kg. The remaining six patients received doses of 1.0, 1.6, 1.8, 1.8, 1.9, and 1.9×106 CAR-positive viable T-cells per kg.
The median time from leukapheresis to product delivery was 15 days, and to product infusion was 27 days, among the 60 efficacy-evaluable patients.
53 of the 60 efficacy-evaluable patients were administered the protocol-defined lymphodepleting chemotherapy regimen of cyclophosphamide 500mg / m² intravenously and fludarabine 30mg / m² intravenously, both given on each of the fifth, fourth, and third days before Tecartus infusion.
The remaining seven patients were either administered lymphodepletion over four days or more or received Tecartus four days or more after lymphodepletion.
All the patients diagnosed were infused with Tecartus on day 0 and were admitted until at least day 7.
The primary measure outcome was objective response rate (ORR) under the Lugano Classification (2014), defined as the incidence of a complete remission (CR) or partial remission (PR) as determined by the independent radiology review committee (IRRC).
In the trial, the objective response rate (ORR) after treatment with Tecartus was 87% with CR rate of 62% and PR rate of 25%.
The most common (≥10%) Grade 3 or higher adverse reactions observed during the trial were thrombocytopenia, anaemia, neutropenia, lymphopenia, leucopenia, encephalopathy, hypoxia, hypophosphatemia, hyponatremia, pyrexia, pneumonia, infection-pathogen unspecified, hypocalcemia, hypertension and hypotension.