Need to know:
- The metaverse has the potential to break down physical and geographical barriers between patients and clinicians. Imagine a patient’s digital twin, outfitted with medical records, meeting clinical trial investigators in a digital world. The metaverse can also be used as an interventional tool to improve patient behaviours.
- Experts warn the clinical trials sector shouldn’t enter the metaverse too quickly due to the need for a solid foundation that guarantees patient and data safety. Virtual reality and telemedicine principles can guide the regulatory framework, but a bespoke approach will be needed.
“Take your time to look around and get used to the height,” a text prompt alerts the virtual reality (VR) user, as the person enters a simulation of being at the edge of a theatre balcony many floors high. As the user’s head moves the visuals follow accordingly, digitally recreating what a person might see in real life.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
This VR tool is for people afraid of heights, as developed by Dr Tara Donker, a principal investigator and co-founder of ZeroPhobia, a low-cost mobile app using VR and augmented reality (AR). Such technology allows patients with phobias to manage their fears without leaving their front door.
The Covid-19 pandemic revealed the potential for wearable technology to shift clinical trials from sites to patient homes. And as technologies continue to improve and become more accessible, software giants are looking to take another leap – into the metaverse.

The metaverse comprises online worlds that people can access through VR headsets and interact with as avatars, explains University of Southern California Institute of Creative Technologies director of medical virtual reality Albert Rizzo, PhD. The metaverse, as recently popularised by Meta (previously known as Facebook) for social gathering, has potential in healthcare where people could enter virtual hospitals, doing away with face-to-face visits, he adds.
The metaverse could be used as a decentralised tool in clinical trials where avatars of doctors and patients meet for a consultation. But it could also be used as a therapeutic tool to improve mental and physical wellbeing.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataWhile intriguing, experts tell Clinical Trials Arena that there is more than meets the eye to ensure patient safety and data protection. It is still unknown how healthcare will fit into the metaverse, and a virtual universe would be a closed world, meaning that not everyone can access it. Rizzo notes that a legal privacy framework regarding data safety, much like Health Insurance Portability and Accountability Act (HIPAA) in the US, would need to be implemented to protect patients.
Metaverse trial to improve youth health
A metaverse can be described as a simulation or a digital universe that uses VR, AR, blockchain, and artificial intelligence (AI), allowing users to interact with each other as avatars. The metaverse is an environment that removes the barriers of travel, time, and cost for people, adds Dr Danny Goel, CEO of PrecisionOS Technology, a Canadian company offering AR and VR for surgical training. “That is a really powerful entity, and it will get better as the time goes on,” he says.
But the role of a metaverse in healthcare is not yet defined, says Dr Ryan Lohre, an orthopedic surgeon who has designed VR research protocols for surgical training. Healthcare and clinical trials, powered by virtual and augmented realities as we know today, will be a part of shaping the sense of how metaverse will fit in the healthcare industry in the future. “Metaverse and healthcare will probably develop at the same rate as it does in other industries,” he adds.
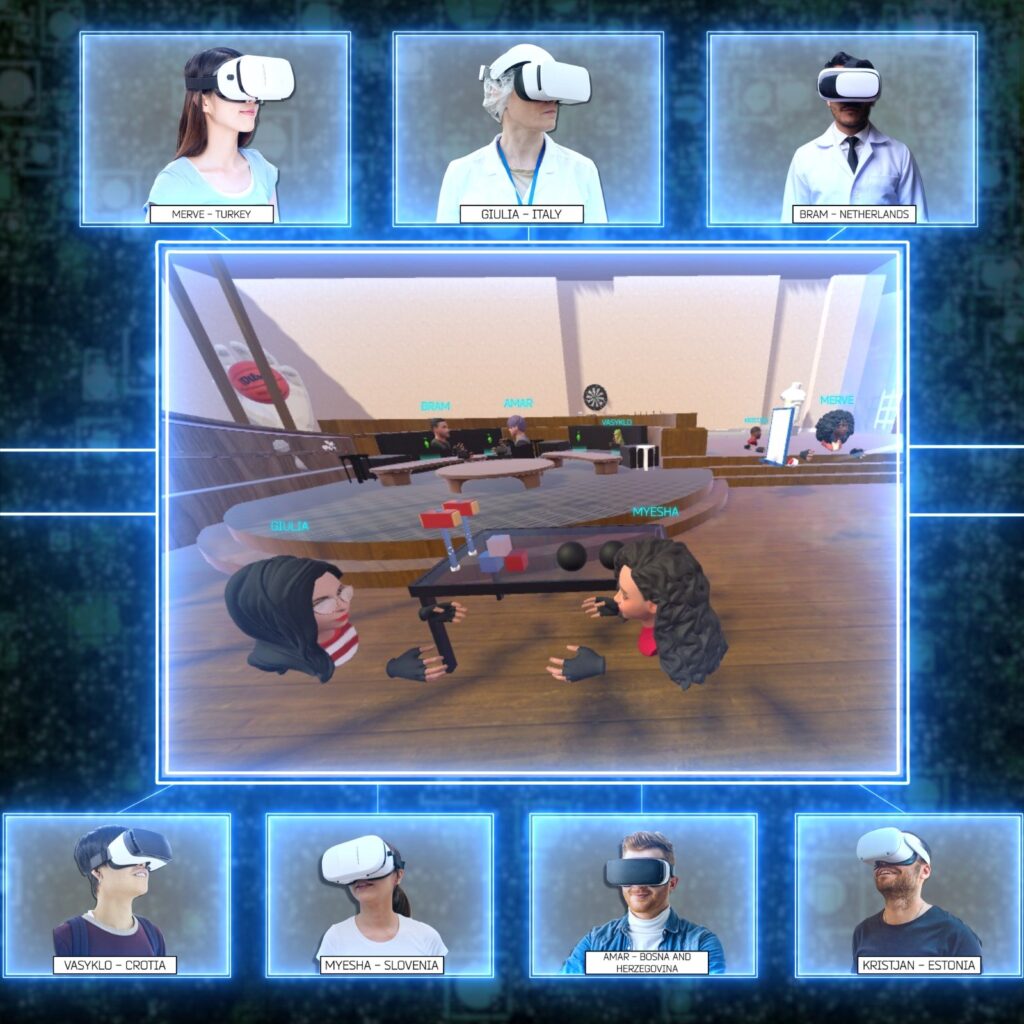
Studies are already being done to test the metaverse as an interventional tool. Akdeniz University paediatric nursing department professor Ayşegül İşler Dalgıç is developing a metaverse-based program, the MetaHealth-Youth Project, to improve healthy behaviours in young people. The multi-country clinical trial (NCT05332886), which is yet to begin, will allow participants to enter three metaverse rooms where they will learn about healthy nutrition, physical activity, and stress management skills to reduce noncommunicable disease (NDC) risk factors.
The study anticipates recruiting 600 students between the ages of 15 and 24. The participants must have a score of 130 or lower on the Healthy Lifestyle Behaviour Scale II (HLBS II) with a body mass index (BMI) level equal to or higher than 25, equivalent to being at least overweight. Students who have chronic or psychiatric disorders, as well as diseases that would prevent the use of metaverse, like vertigo, are excluded.
Dalgıç explains that the younger generation’s interest in technology may mean that metaverses will be widespread in the future, thus using such a platform will sustain the innovative approaches in health and education systems. Two other trials using a metaverse-assisted home monitoring model in ophthalmology are listed on ClinicalTrials.gov, with both studies based in China.
Metaverse: telemedicine to the next level?
A digital simulation where people can interact with each other open possibilities in healthcare, including clinical trials. “The volume of social and behavioural studies that could be explored are significant,” Goel adds. Metaverses offer an opportunity to run clinical trials at scale with minimal cost, as it allows investigators to access many people and gather a lot of insight in a short period of time, he explains.
Much like telemedicine, a physician would meet the patient virtually, but in this case, as a 3D simulation. The patient would be represented as an avatar, a digital twin based on the patient’s electronic medical record (EMR).
However, assessing symptoms through an avatar is not suitable for all areas of medical care, Donker says. For example, in mental health, physical appearance, hygiene, and even eye gaze are important aspects to determine if a patient is taking care of themselves. The removal of the human element could cause more harm than good, as physicians assessing the patient can miss a lot of very important information to base their diagnosis and treatment, Donker adds. In dermatology, assessment of skin problems is challenging as it is with existing telemedicine technologies due to video quality issues.
Dalgıç highlights that in his MetaHealth-Youth Project trial, avatars will be created for users to interact, talk, and perform physical activities with each other, not for diagnostic purposes.
Patient safety on the forefront
Another key consideration is how the metaverse would pass through regulatory requirements. It must go through proper regulatory capacity to ensure it is safe, secure, private, and respect patient autonomy, Lohre says, “we can’t let industry get ahead of regulators.”
If digital universes are used in healthcare, developers must respect current recommendations around clinical trials and ethics behind it, including patient consent and monitoring. Delineating who can consent for adolescent patients is also a priority, Lohre notes.
As telemedicine and VR are in the same family, those regulations could apply to metaverses, Rizzo says. Yet, extra precautions and research need to be taken to ensure that metaverse technology is safe for patients. He adds: “We have to take small steps to make sure we can ensure safety, that a bunch of hackers can’t come in and have a field day watching people suffering.”
The MetaHealth-Youth Project is a closed world, only accessible to the study participants to ensure their safety and protection of the personal and health data, Dalgıç says. However, since metaverse as a healthcare concept is still in its infancy, it is hard to tell how accessibility will work once other metaverses launch for the public.
Lohre says that even traditional trials recruiting across multiple countries is already a challenge, as every country has different data protection laws. Creating a virtual space where people can enter from different regions will add extra data protection challenges. “It is going to take a lot of collaborative work between a lot of different regulatory authorities to be able to do that,” he adds.
Exposure therapy using virtual environments
While how the metaverse can be used in trials or if it can be used as a therapeutic approach is yet to be fully defined, the tools to get there are already being used. In fact, VR tools in mental health have been around for longer than one would expect. Donker started her research on VR and mental health in 2006, but first studies were already being done in the mid-90s.
VR allows the user to enter a virtual environment through a headset, while AR implements virtual components in the real-world environment. These technologies allow the user to be in control of the virtual space, which is a beneficial tool for phobia-related exposure treatments, Donker says.
As an example of AR as a therapeutic tool, Donker will be leading a 112-participant study in a 10-level AR treatment for the fear of spiders. The patient chooses a spider, whether it’s a cellar spider or a more intimidating tarantula, to interact with. In the first level, the patient decides the movement of the spider, but with each level the insect gains more autonomy. In the final level, the patient sees a mother spider crawling over the table with its babies in tow.

While the trial protocol is under revision, the randomised, wait list-controlled trial is to investigate if the tool ZeroPhobia offers any improvements after six weeks, as measured via the Fear of Spider Questionnaire. Virtual simulation does away with traditional exposure therapies, such as real-life animals or insects that cannot be controlled, Donker notes. Phobias like thunder, lighting, or flying on a plane are much more complicated to replicate in the real word, showing another benefit of virtual interventions.
A total of 20 Phase I–III trials are ongoing or planned investigating different methods of treatment for various phobias, according to GlobalData’s Clinical Trial Database. GlobalData is the parent company of Clinical Trials Arena.
Nevertheless, introduction of any new technology such as the metaverse will have early challenges. But the goal is to make the metaverse an opportunity for healthcare to move beyond its current state, Goel notes. Healthcare has been based on tradition, and this is a chance to think beyond that, initially abstractly, but in the future in a more concrete way, he adds.
The concept of a digital universe, maybe even multiple, sounds futuristic — ripped out of a science fiction novel or a computer game. The opportunity to break down physical and geographic barriers to explore a collaborative world is seductive; but before we reach such a utopian vision, solid foundations must first be built to protect the scientific process and what matters the most: the real world patient.





