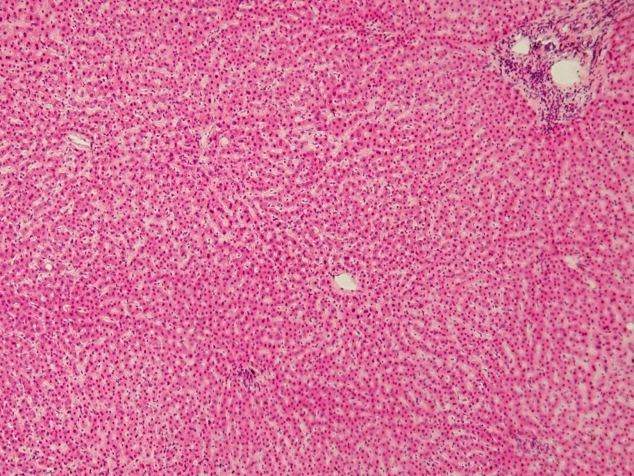
A new study by researchers at the Stanford University School of Medicine has reported liver cells with high levels of the protein telomerase enable the organ’s regeneration during normal cellular turnover or tissue damage.
Results from the study support the hypothesis of a ‘distributed model’ of liver cell (hepatocyte) renewal, where a subset of hepatocytes dispersed throughout the lobule replicates and expands to maintain liver mass. The research team found liver stem cells dispersed throughout the organ’s lobes, enabling its rapid repair regardless of where damage occurs.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The trial was conducted in mouse models, with findings published in Nature.
Telomerase is a protein complex generally associated with aging resistance, and is found at the ends of chromosomes following DNA replication. Without it, protective chromosomal caps known as telomeres would shorten with each cell division.
The majority of adult cells have little or no telomerase activity, and the progressive shortening of their telomeres gradually limits the cells’ life span. Mutations in telomerase pathway genes have previously been found to cause liver diseases.
Stem cells make enough telomerase to prevent the shortening of telomeres, allowing for almost unlimited cell division. Certain cancer cells also have this ability, and some mutations that increase telomerase are commonly found in liver cancers. Conversely, mutations which block telomerase activity are known to cause cirrhosis.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe researchers attempted to use telomerase expression to identify the subset of cells responsible for regenerating the liver during normal turnover. These cells could also serve as the origin cell for liver cancer.
Lead author Dr Shengda Lin found that in mouse models around 3% to 5% of all liver cells expressed abnormally high levels of telomerase, as well as low levels of the genes found in normal cellular metabolism. These cells were distributed evenly throughout the organ’s lobules, though during regular cell turnover or following damage they collected in certain areas to form clusters of new liver cells.
“These rare cells can be activated to divide and form clones throughout the liver,” said the Stanford study’s senior author Dr Steven Artandi.
“As mature hepatocytes die off, these clones replace the liver mass. But they are working in place; they are not being recruited away to other places in the liver. This may explain how the liver can quickly repair damage regardless of where it occurs in the organ.”
As the stem cells were found to express fewer metabolic genes, the results could provide a means of limiting the production of metabolic by-products which damage DNA.
“This may be one way to shelter these important cells and allow them to pass on a more pristine genome to their daughter cells,” Artandi said.
“They are not doing all the ‘worker bee’ functions of normal hepatocytes.
“You could imagine developing drugs that protect these telomerase-expressing cells, or ways to use cell therapy approaches to renew livers. On the cancer side, I think that these cells are very strong candidates for cell of origin. We are finally beginning to understand how this organ works.”
Lin also engineered the telomerase-expressing hepatocytes to die in response to a chemical signal and gave the mice a liver-damaging chemical. He found that the mice in which the telomerase cells had been killed exhibited much more severe liver scarring than those in which the cells were functional.
The liver is the only one of the body’s organs to be able to regenerate from as little as 25% of its original mass. Currently, little is known about the cellular cause of liver regeneration and which of its cells aid the development of cancer.
“The liver is a very important source of human disease,” Artandi said.
“It’s critical to understand the cellular mechanism by which the liver renews itself. We’ve found that these rare, proliferating cells are spread throughout the organ, and that they are necessary to enable the liver to replace damaged cells. We believe that it is also likely that these cells could give rise to liver cancers when their regulation goes awry.”
Gaining insight into the process of repair would enable greater understanding of what happens in diseases such as cirrhosis or liver cancer, when the organ loses normal functionality. The former condition causes around 900,000 deaths worldwide every year, while the latter is the fifth most common cause of cancer-related death in the US.
The liver can also be damaged through chronic alcoholism or hepatitis infection, both of which can cause scarring which inhibits the organ’s normal cycle.





