Krazati™ (adagrasib) is a highly selective, small molecule, RAS GTPase family inhibitor indicated for the treatment of adult patients with Kirsten Rat Sarcoma (KRAS)G12C mutated locally, and advanced or metastatic non-small cell lung cancer (NSCLC), who have received at least one prior systemic therapy.
Developed by US-based biotechnology company Mirati Therapeutics (Mirati), Krazati was approved by the FDA in December 2022. It is the second KRAS inhibitor to receive US Food and Drug Administration (FDA) approval for advanced, previously treated NSCLC, after Amgen’s KRAS inhibitor Lumakras (sotorasib), which was approved in May 2021.
Krazati is available as immediate-release, oval-shaped, white-to-off-white film-coated tablets in 200mg dosage strength for oral administration. Mirati markets the drug via Onco360®, an independent speciality pharmacy in the US.
The drug is being studied both as a monotherapy and in combination with other anti-cancer drugs in patients with advanced KRASG12C-mutated solid tumours such as NSCLC, colorectal cancer and pancreatic cancer.
Companion diagnostics to identify KRASG12C mutation
Mirati and US-based diagnostics company Agilent developed Agilent Resolution ctDx FIRST, a liquid biopsy companion diagnostic test. In addition, Mirati collaborated with QIAGEN, a biotechnology company based in Germany, to develop a tissue-based Therascreen® KRAS RGQ PCR kit. Both tests identify patients with KRASG12C mutations.
The two companion diagnostics received FDA approval for the use of Krazati in the treatment of advanced NSCLC in December 2022, along with the accelerated approval of the drug itself for the same condition. Patients identified as eligible by an FDA-approved companion diagnostic test can now receive the therapy.
Regulatory approvals for Krazati
In June 2021, Adagrasib received breakthrough therapy designation from the FDA for the potential treatment of patients with NSCLC who had the KRASG12C mutation and who had received previous systemic therapy.
The FDA accepted the new drug application (NDA) for adagrasib for this condition submitted by the company in February 2022.
In May 2022, Mirati filed a marketing authorisation application (MAA) to the European Medicines Agency (EMA) for adagrasib for the treatment of previously treated NSCLC patients with KRASG12C mutation.
Krazati also holds fast-track and orphan drug designations from the FDA for the treatment of patients with NSCLC.
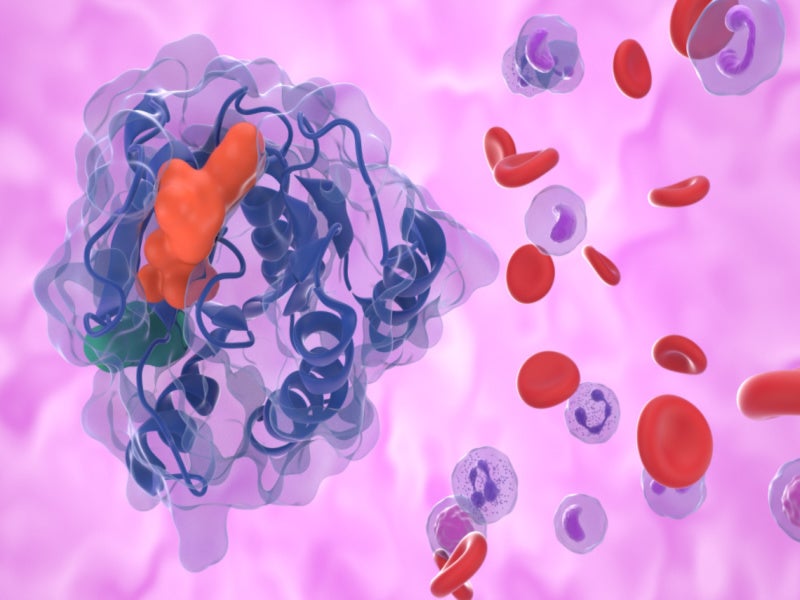
Non-small cell lung cancer causes
Lung cancer is one of the most frequent cancers in the world, with 2.21 million new cases and 1.8 million deaths recorded in 2020.
Lung cancer is mainly of two types. Histologically these are NSCLC, which accounts for about 85% of lung cancer cases, and small cell lung cancer (SCLC), which accounts for 15% of cases.
KRAS serves as an on-and-off switch for cell growth and instructs a cell to stop growing in normal conditions. When KRAS is mutated, the cells continue to grow abnormally and often develop into some of the most aggressive cancers. KRASG12C is the most common KRAS mutation in NSCLC, occurring in approximately 14% of patients with NSCLC.
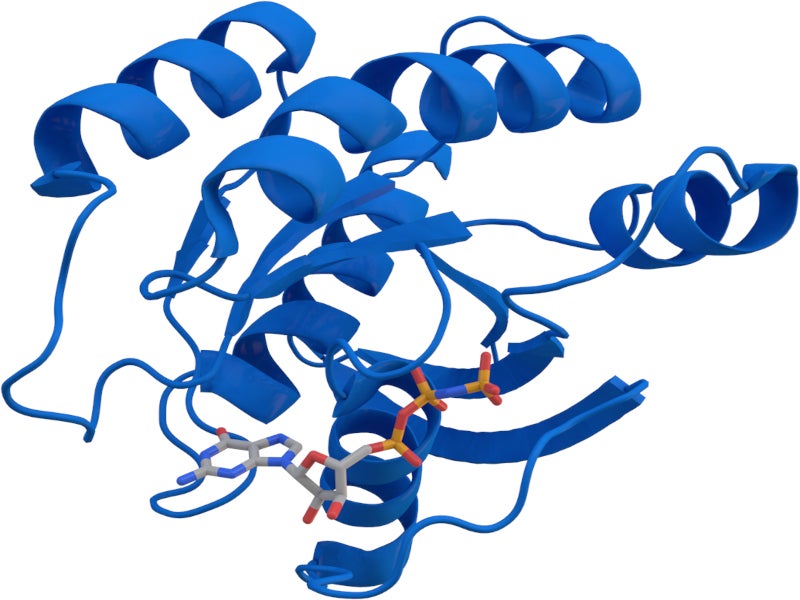
Krazati’s mechanism of action
Krazati is a highly selective, potent and irreversible inhibitor of KRASG12C that covalently binds to the mutant cysteine in KRASG12C and locks the mutant KRAS protein in an inactive state, preventing downstream signalling without altering the wild-type KRAS protein.
The drug blocks tumour cell growth and viability in KRASG12C-mutated cells. It resulted in tumour regression in KRASG12C-mutated tumour xenograft models with negligible off-target activity.
Clinical trials on Krazati
The FDA’s accelerated approval of Krazati was based on results from a multi-centre, single-arm, open-label expansion cohort clinical trial named KRYSTAL-1.
In the study, the drug’s efficacy was assessed in 112 eligible patients with locally advanced or metastatic NSCLC with KRASG12C mutations, whose disease had progressed either during or after platinum-based chemotherapy and an immune checkpoint inhibitor, administered either concurrently or sequentially.
Patients were given adagrasib 600mg orally twice a day until they exhibited signs of unacceptable toxicity or disease progression. Tumour development was evaluated every six weeks.
The primary efficacy outcome measures were confirmed objective response rate (ORR) and duration of response (DOR), as determined by a blinded independent central review (BICR) using response evaluation criteria in solid tumours (RECIST v1.1).
The patients achieved an ORR of 43% with 80% of them achieving disease control. The median DOR was 8.5 months.
The most common side effects reported in patients in the clinical trial included diarrhoea, nausea, tiredness, vomiting, musculoskeletal pain, hepatotoxicity, renal impairment, dyspnoea, oedema and reduced appetite.