
After a busy two-day discussion about what needs to be done to improve the UK’s contribution to clinical trials, there seems to be a light at the end of the tunnel.
The 10th annual Arena Internationals Outsourcing in Clinical Trials UK and Ireland 2023 (OCT23) conference was held in London on 5 and 6 September 2023, where big and small pharma, regulatory, health charities, site staff, data software providers and more came together to discuss clinical trials in the UK.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The conference was pinned on the fact that there has been a 44% drop in clinical trials initiated in the UK over the last five years, taking the UK from 4th to 10th in regard to global contribution – a bit of a hit for the country. Despite this, doctors have spoken about their wish to conduct research and patients have spoken about their desire to be involved in research, signalling a move in the right direction.
Those in attendance at OCT23 have hopes for the future but highlighted that an extraordinary amount of changes need to be made for easier conduct of trials in the country, providing a more attractive trial landscape for pharma.
Primary care could be the answer but GPs do not have time
The event was opened with a keynote speech by Professor Lucy Chappell, chief scientific advisor of the Department for Health and Social Care, about the future of UK clinical research. Chappell spoke about how the government has reflected on a report published by Lord James O’Shaughnessy, who spoke on the second day of the conference. The report pushes for primary care to become more involved in clinical research including general practitioners (GPs). Chappell says that bringing research into GP surgeries makes it much easier to ensure patients can access cutting-edge therapies.
“The potential is there are better patient outcomes, better for the workforce, better for the system. Who wouldn’t want to have research embedded in their practice?” Chappell asks.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataQuestions were asked about the availability of GPs to take part in research after a Royal College of Physician survey found that 57% of NHS doctors want to participate in research, but 53% cited time constraints as the biggest barrier to research participation. Chappell adds that this move does not mean all GPs must be directly involved in research but just signposting patients to research will be an improvement.

“You’ve got three options: you can be research aware, you can be research active or you can be a research leader.” The option that isn’t on the table is to be a research blocker. You can’t stop it from happening,” Chappell says. “If we brought everyone to even the first level of instruction where they signpost patients to that research, is that so hard?”
Lord O’Shaughnessy’s talk reflected on his report and spoke about what changes have been acted on since its publication. O’Shaughnessy says that he understands the difficulties that GPs are facing and that he maybe should have pushed further for designated time in a doctor’s schedule to be involved in research.
“Saying, well, we’re going to magically save 5% of a GPs time and set it aside without some other big change, I just think is potentially unrealistic,” O’Shaughnessy notes. “Albeit, that is something we have to grapple with.”

O’Shaughnessy spent hours conversing with industry while compiling his report and he mentioned that one person asked why they could not just go back to how the landscape was five years ago. The Clinical Trials Arena asked O’Shaughnessy what he hopes to see from the UK’s clinical trial contributions in five years.
“We will have doubled and then doubled again, our commercial clinical trial activity. O’Shaughnessy says. “There’s no reason we can’t do that.”
Inspiring talks from all parts of the industry
There were dozens of other speakers at the event but some standout talks included Bob Stevens, Group CEO of the MPS Society, Abi Hunter, senior director head of clinical sampling at AstraZeneca, Dr Ian Bruce, NIHR Manchester Biomedical Research Centre, and Dr Suki Balendra, director of strategic partnerships at Paddington Life Sciences and Neelam Patel, non-executive director of the Health Research Authority (HRA).
Stevens spoke about his two sons, diagnosed at a young age with Mucopolysaccharidosis type II (MPS II) – known as Hunter Syndrome. Following their diagnosis, he has had to be a patient advocate for them throughout their lives and set up the MPS society so he can advocate for other patients with rare diseases to be involved in clinical trials.
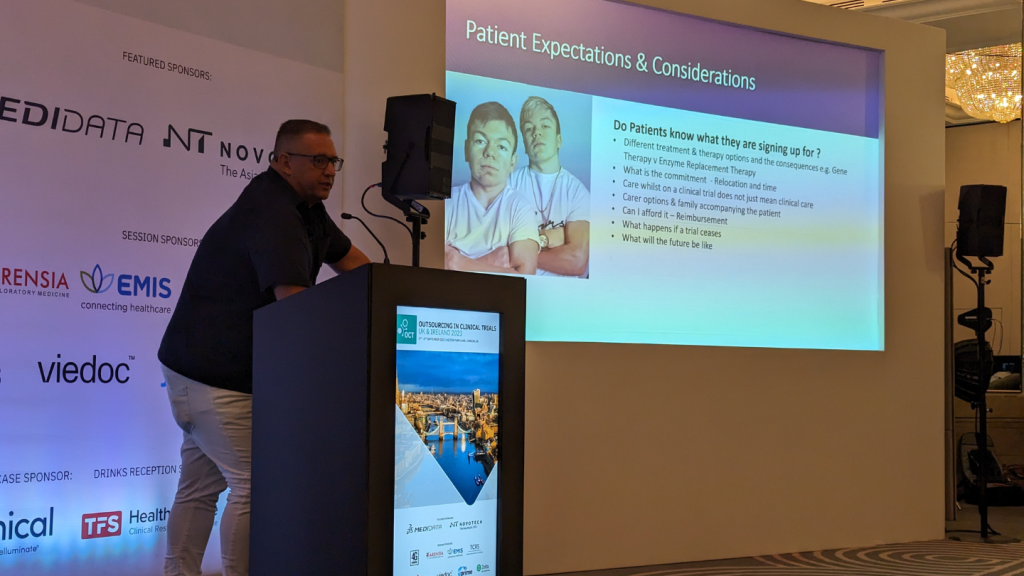
“We are patient families, we are patient organisations, we understand our patients better than anyone else,” Stevens explains. “Everything we make goes straight back to our patients.”
Hunter spoke about how AstraZeneca has big ambitions to be carbon-negative by 2030 including in its clinical sampling operations. Hunter spoke about how the company is working with green transportation, reducing plastic by looking at the possibility of multi-use kits, taking one large blood sample from a patient rather than several smaller samples and only testing when necessary during a trial.
Hunter added that she hopes that by sharing the techniques that AstraZeneca is utilising other big and small pharma may also take accountability for their carbon footprint. “There’s no reason that all these things we’re doing can’t be industry-wide,” Hunter explains. “There’s a real opportunity here as an industry to really drive change as a whole.”
Bruce spoke about the Greater Manchester model after the borough bucked the trend of reducing clinical trial research with a 44% increase in patients from 2017 to 2018 to 2021 to 2022. Greater Manchester also beat national average times of study set up, of an average of 51 days compared to the national median of over 117 days since 2019.

Dr Suki Balendra and Neelam Patel discussed the ongoing issue of diversity in clinical trials. The pair discussed how earlier this year, the HRA published guidance about improving diversity in clinical research, which includes a number of steps the HRA is taking itself. One way that Dr Balendra and Ms Patel recommended improving trust in the community is for CROs and sponsors to have a more diverse staff and key opinion leaders to ensure people feel represented.
Patel notes: “We recommended that research institutions, funders and companies should think about their workforce and encourage recruitment from diverse populations and training to support their staff to do that.”

Panel conversations and fireside chats
Some of the most insightful conversations of the event came from the panels talks about other concerns for the UK industry, including whether technology is being properly utilised in trials and what needs to be done to improve the UK’s clinical trial infrastructure.
In a panel conversation on 5 September, Krzysztof Potempa, founder and CEO of Braincures, Marin Ebudor, clinical lead for digital transformation at NHS East London, Marisa Papaluca, expert medicines regulatory advisor, and Greig Duncane, solution sales specialist of clinical operations at Medidata, spoke about whether technology is being utilised enough in clinical trials.
The consensus was rather negative but with hopes of a better future. Ebudor mentioned how during clinical practice, he has not seen medical devices in trial being utilised. “In the general healthcare space, as a frontline clinician myself I have not seen much of this new wider technology trickled down onto the frontline,” Ebudor explains. “I see lots of interesting things in other industries happening but in healthcare, often it takes a long time to see some of those things appear for various reasons such as regulation.”
A second panel held on 6 September included Bruce, Dr Janet Messer, director of approvals service at the HRA, Oliver Buckley-Mellor, innovation and research policy manager at the Association of the British Pharmaceutical Industry, and Alison McMorn VP of clinical development at AMO Pharma. The panel discussed the state of the UK infrastructure for trials and improvements needed to make the country a top contributor again. One of the biggest issues raised by the panel was the MHRA’s backlog with registering clinical trials.

McMorn spoke about how this has made Pharma struggle to initiate trials in the UK compared to other countries making it a less inviting country for pharma to host trials. “It’s been really tough. I don’t think we can underestimate what impact the difficulties that we have been facing with the MHRA have had on us.”
There was a great deal of interesting conversation during OCT23 which highlighted a number of issues in the UK’s clinical trial industry but it is not all doom and gloom. With Lord O’Shaughnessy’s report and improvements in regulatory bodies such as the MHRA, it appears that it will become easier for trial initiation in the UK. Hopefully, at next year’s conference, there will be a much more positive outlook for the future.





