HYQVIA® (immune globulin infusion 10%) is a liquid medicine that combines immune globulin infusion at a 10% concentration with the recombinant human hyaluronidase PH20 (rHuPH20) enzyme, for the treatment of primary immunodeficiency (PI) and chronic inflammatory demyelinating polyneuropathy (CIDP).
The drug was originally developed by Baxter International and was first launched in Europe in 2013. Shire gained HYQVIA after it acquired Baxter in June 2016. The drug subsequently became part of Takeda Pharmaceutical’s portfolio, following its acquisition of Shire in January 2019.
HYQVIA utilises the ENHANZE® drug delivery technology developed by Halozyme, a biopharmaceutical company in the US. The technology facilitates the removal of a barrier for fluid flow, enabling the administration of large-volume subcutaneous (SC) injections that can be dispersed and absorbed more effectively.
HYQVIA is an SC immunoglobulin treatment that can be administered once a month. It serves as a replacement therapy for primary and certain secondary immunodeficiencies.
HYQVIA is a dual vial unit, with one vial containing 100mg/ml of immune globulin infusion 10% (human) and the other comprising 160U/ml of rHuPH20. HYQVIA is available in a range of vial volumes, including 25ml, 50ml, 100ml, 200ml and 300ml, to accommodate varying dosage requirements.
Regulatory approvals for HYQVIA
The US Food and Drug Administration (FDA) approved HYQVIA as a maintenance therapy for CIDP to prevent relapse of neuromuscular disability and impairment in adults in January 2024. The approval was based on the outcomes of the phase III ADVANCE-CIDP 1 and ADVANCE-CIDP 3 clinical trials.
HYQVIA received authorisation in Europe in the same month as maintenance therapy in CIDP patients of all ages, following stabilisation with intravenous immunoglobulin therapy (IVIG). HYQVIA was granted marketing authorisation by Health Canada in January 2022.
HYQVIA was initially approved in the US in September 2014 for PI in adults and its indication was later expanded to include paediatric patients aged from two to 16 years.
HYQVIA for paediatric use was launched by Shire in Europe in July 2016.
The European Commission approved HYQVIA for the treatment of PI in 2013 and secondary immunodeficiency (SID) in 2020. The product is also licensed in Puerto Rico and Australia.
Primary immunodeficiency causes and symptoms
PI involves a group of more than 400 rare, chronic disorders that impair the normal functioning of the immune system. The disorders are mostly hereditary, although some can arise from a combination of genetic and environmental factors.
The immune system’s primary role is to protect the body against pathogenic microorganisms that can cause infectious diseases. When an individual’s immune system is dysfunctional, they become more vulnerable to infections and may experience prolonged recovery periods. Primary immune deficiency arises when the defect in the immune system is of genetic origin.
The symptoms of PI disorders are diverse and can include pneumonia, bronchitis, sinus infections, ear infections, meningitis or skin infections. Individuals may suffer from inflammation of internal organs, blood disorders, digestive problems, delayed growth and development and autoimmune disorders such as lupus, rheumatoid arthritis and Type 1 diabetes.
An estimated six million individuals globally are affected by primary immunodeficiencies.
Chronic inflammatory demyelinating polyneuropathy causes and symptoms
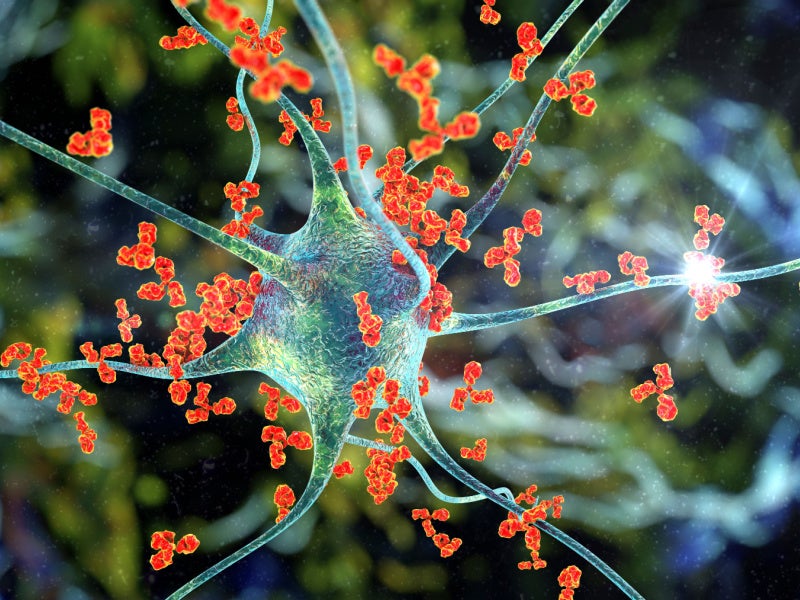
CIDP is a rare acquired autoimmune disorder that targets the peripheral nervous system. The condition is characterised by the immune system’s attack on the myelin sheaths surrounding nerve cells, although the precise cause for this autoimmune response remains unclear.
Symptoms of CIDP are generally consistent, regardless of the subtype, and are characterised by progressive, symmetrical symptoms, such as muscle weakness, tingling or numbness in the limbs, gradual weakening of the arms and legs, loss of reflexes, balance difficulties and challenges with walking.
HYQVIA’s mechanism of action
HYQVIA is a therapeutic formulation, combining immune globulin with recombinant human hyaluronidase.
The Immune Globulin Infusion is a 10% solution derived from large human plasma pools, which account for at least 98% of immunoglobulin G (IgG) in its composition with a wide array of antibodies that contribute to the therapeutic efficacy of HYQVIA.
Recombinant human hyaluronidase of HYQVIA serves to increase the distribution and absorption of the immune globulin infusion within the subcutaneous layer between the skin and muscle. It is achieved through the enzymatic activity of hyaluronidase on hyaluronan, a polysaccharide prevalent within the extracellular matrix of connective tissues.
Hyaluronan is characterised by its rapid turnover rate in the body, with a half-life of approximately 0.5 days, and is depolymerised by the naturally occurring enzyme hyaluronidase. The rHuPH20 present in HYQVIA temporarily increases the permeability of the subcutaneous tissue by depolymerising hyaluronan. The action facilitates the dispersion and subsequent absorption of the immune globulin, ensuring that the medication is effectively delivered to the patient’s system.
The effects of rHuPH20 are localised and temporary, with the normal permeability of the subcutaneous tissue restored within a period of 24 to 48 hours post-administration.
Clinical trials on HYQVIA
The findings from the phase III ADVANCE-CIDP 1 and ADVANCE-CIDP 3 clinical trials have been pivotal in establishing the efficacy of HYQVIA as a maintenance therapy for CIDP.
The ADVANCE-CIDP 1 trial was a multi-centre, placebo-controlled, double-blinded study aimed at evaluating the efficacy, safety and tolerability of HYQVIA with recombinant human hyaluronidase as a maintenance therapy to prevent relapse in CIDP. The trial included 132 adults who had received a confirmed CIDP diagnosis and had been on a stable intravenous immune globulin (IVIG) therapy dosing regimen for a minimum of three months before the screening process.
The primary endpoint of the study was to measure the proportion of participants who experienced a worsening functional disability. It is defined as an increase greater than or equal to one point relative to the pre-subcutaneous treatment baseline score in two consecutive adjusted Inflammatory Neuropathy Cause and Treatment disability scores.
The primary efficacy analysis involved a comparison of relapse rates, using a continuity-corrected χ2 test at a 5% level of statistical significance, and missing data were assumed to represent no relapse.
Participants in the trial were randomised to receive either HYQVIA or a placebo, administered at the same dosage and frequency as their previous IVIG treatments, for six months or until a relapse occurred. Those who experienced a relapse were then provided with IVIG as a rescue therapy for up to six months.
The results from the ADVANCE-CIDP 1 trial showed a significant reduction in the relapse rate of CIDP observed in the HYQVIA group compared to the placebo group, which was 15.5% versus 31.7%, respectively.
The analysis of the primary endpoint revealed a statistically significant difference in relapse rates between the HYQVIA group (14.0%) and the placebo group (32.3%), with a treatment difference of -18.3%, demonstrating the superiority of HYQVIA in preventing CIDP relapses.
Following the initial trial, participants who did not experience a relapse were allowed to continue treatment with HYQVIA in the subsequent ADVANCE-CIDP 3 trial. The open-label extension trial was designed to evaluate the long-term safety, tolerability and immunogenicity of HYQVIA in patients with CIDP who had completed the ADVANCE-CIDP 1 trial.
The most common adverse reactions reported by participants were local reactions, headaches, fever, nausea, fatigue, erythema, itching, increased lipase levels, abdominal pain, back pain and pain in extremities.