PiaSky® (crovalimab) is an anti-complement C5 monoclonal antibody indicated for the treatment of paroxysmal nocturnal haemoglobinuria (PNH), a rare and life-threatening blood condition.
It is eligible for paediatric and adult patients aged 12 years and older with a body weight of at least 40kg.
The drug was developed by Chugai Pharmaceutical, a pharmaceutical company based in Japan, and a subsidiary of Roche Group. PiaSky uses Chugai’s Recycling Antibody® technology, enabling subcutaneous administration at low doses once every four weeks.
PiaSky is available as a clear to opalescent, almost colourless to brownish-yellow solution in a single-dose vial in 340mg/2ml (170mg/ml) dosage strength for intravenous or subcutaneous administration.
Regulatory approvals for PiaSky
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) recommended crovalimab for the treatment of PNH in adults and adolescents aged 12 and above in June 2024, based on the results of the global Phase III COMMODORE 2 clinical trial.
The US Food and Drug Administration (FDA) accepted a biologics licence application for crovalimab in September 2023, leading to its approval in June 2024 for the treatment of PNH in adults and adolescents aged 13 years and older. The drug is made available to patients in the US by Genentech, a subsidiary of Roche.
In Japan, Chugai Pharmaceutical filed a new drug application for PiaSky with the Japan Ministry of Health, Labour and Welfare (MHLW) in June 2023. The drug was approved in March 2024 and subsequently launched in May 2024 for patients with PNH aged 12 years and above.
In February 2024, China’s National Medical Products Administration (NMPA) approved crovalimab for the treatment of PNH in adults and adolescents aged 12 years and older without prior complement inhibitor treatment, following a priority review initiated in August 2022.
PiaSky is also under review by other regulatory authorities, including those in Europe and Taiwan.
Paroxysmal nocturnal haemoglobinuria (PNH) causes and symptoms
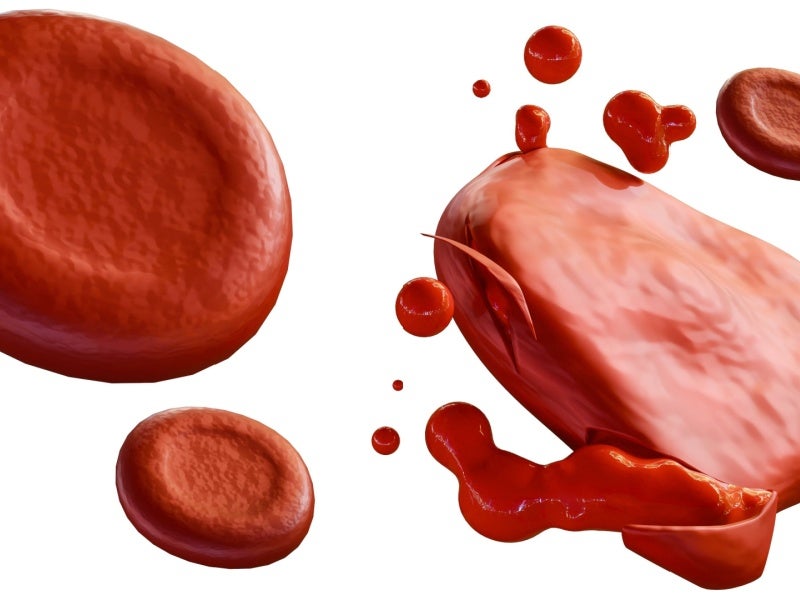
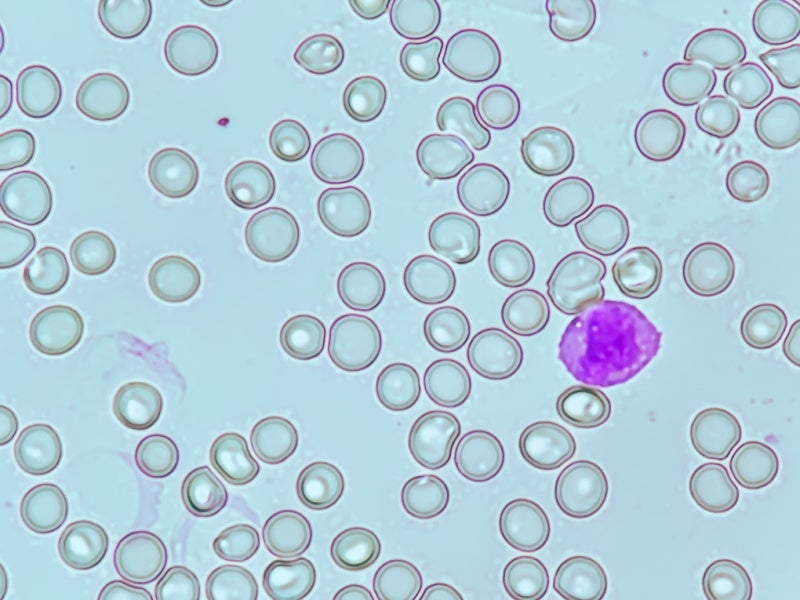
In PNH, red blood cells are targeted for destruction by the complement system, a component of the body’s innate immune response. The process results in symptoms such as anaemia, fatigue, and blood clots, and can even progress to kidney disease and pulmonary hypertension.
Symptoms vary but typically include haemoglobinuria and thrombosis due to haemolysis, and similar haematopoietic failures as those seen in aplastic anaemia.
The disease affects approximately 20,000 people worldwide.
PiaSky’s mechanism of action
Crovalimab is a C5 inhibitor that is recycled within the bloodstream and binds with high affinity to the complement protein C5, inhibiting its cleavage into C5a and C5b and preventing the formation of the membrane attack complex (MAC). This action inhibits terminal complement-mediated intravascular haemolysis in patients with PNH, delivering rapid and sustained complement inhibition.
Chugai’s recycling antibody technology details
Chugai’s proprietary Recycling Antibody technology enables the development of antibodies that can bind with an antigen multiple times, thus offering prolonged efficacy compared to conventional antibodies. This is achieved by engineering antibodies to dissociate from the antigen at an acidic pH within the endosome.
The technology is used in PiaSky, making it the second FDA-approved product following Enspryng® (satralizumab) to do so. Multiple antibodies using this technology are currently undergoing clinical studies and drug discovery processes.
Clinical trials on PiaSky
The COMMODORE 2 study, a Phase III open-label, active-controlled, non-inferiority, randomised clinical trial, was pivotal in the FDA’s approval of PiaSky.
The trial compared the efficacy and safety of PiaSky with eculizumab in 204 patients with PNH who had not been previously treated with a complement inhibitor. Patients were randomised in a 2:1 ratio to receive either PiaSky every four weeks or intravenous eculizumab every two weeks. The study had a primary treatment period of 24 weeks.
The co-primary efficacy endpoints of the study were transfusion avoidance and control of haemolysis, with additional endpoints, including breakthrough haemolysis and stabilised haemoglobin levels. The results demonstrated that PiaSky was comparable to eculizumab in these measures, with 65.7% of patients treated with PiaSky avoiding transfusion compared to 68.1% for eculizumab, and 79.3% of PiaSky-treated patients achieving haemolysis control compared to 79% for eculizumab.
Furthermore, the study included a separate non-randomised cohort of six paediatric patients aged above 12 years with a body weight greater than or equal to 40kg, receiving PiaSky. The efficacy in paediatric patients was consistent with that observed in adults, as evaluated in COMMODORE 2.
The treatment effect of PiaSky in paediatric patients with PNH was found to be consistent with that observed in adults with PNH.
The most common adverse reactions observed were infusion-related reactions, respiratory tract infections, viral infections, and Type III hypersensitivity (T3H) reactions.
Additional clinical trials on PiaSky
COMMODORE 1 is a Phase III, randomised, open-label, active-controlled clinical trial evaluating crovalimab versus eculizumab in complement inhibitor–experienced patients with PNH. The study enrolled adult patients with PNH for a primary treatment period of 24 weeks.
COMMODORE 1 demonstrated that crovalimab is well tolerated in patients with PNH who have prior experience with C5 inhibitors. Its safety profile is consistent with that observed in C5 inhibitor-naive patients, except for the risk of transient T3H reactions when switching between inhibitors targeting different C5 epitopes.
Patients transitioning from eculizumab to crovalimab maintained disease control, supported by complete and sustained C5 inhibition with crovalimab.
These findings, along with the results from Phase III COMMODORE 2, underscore the favorable benefit–risk profile of crovalimab.
Additionally, PiaSky is also being evaluated for the treatment of atypical haemolytic uremic syndrome (aHUS), sickle cell disease (SCD) and lupus nephritis.