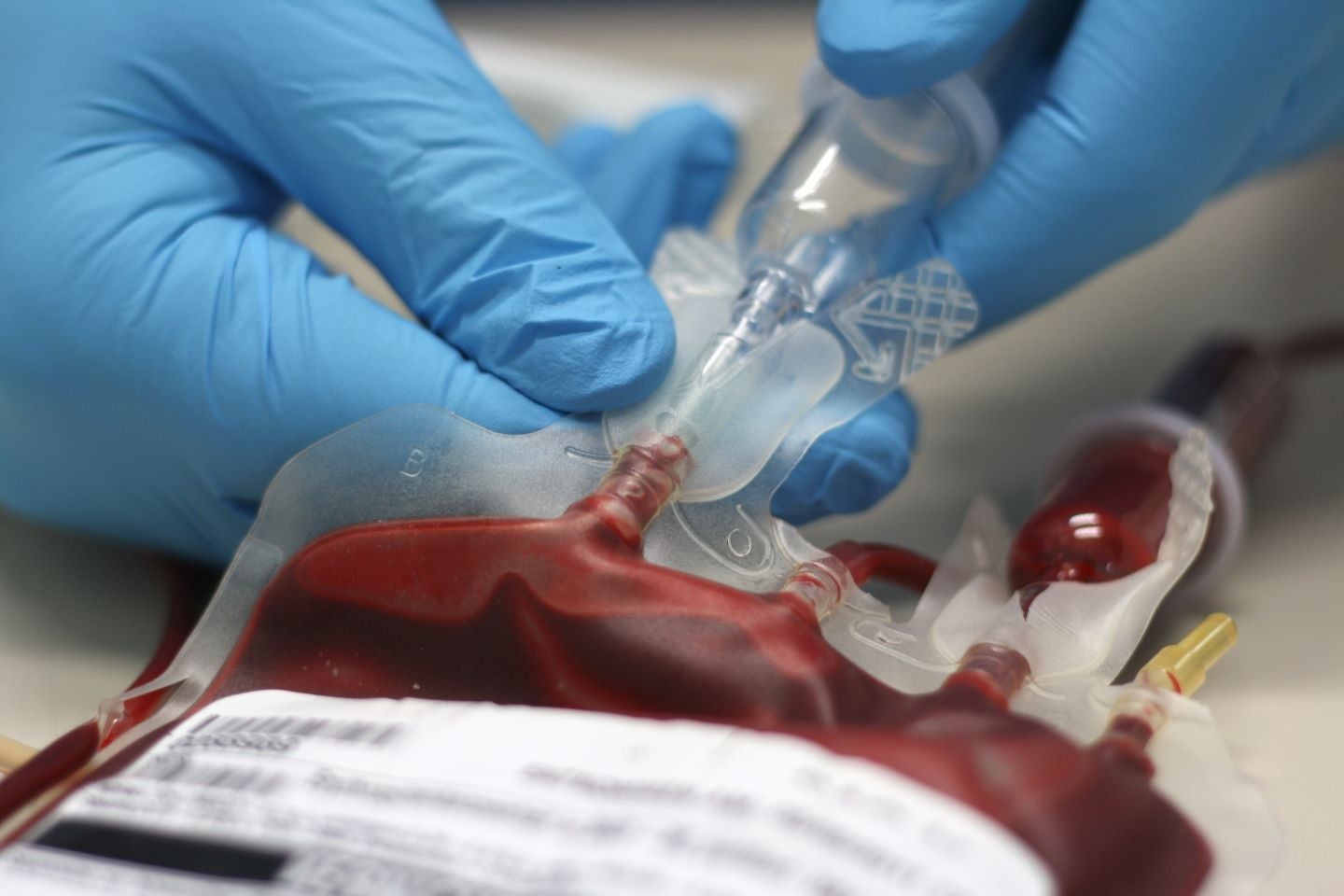
According to the National Institute for Health and Care Excellence (NICE), sickle cell disease, a group of inherited diseases that act on red blood cells, affects one in every 2,000 live births in England. The diseases can vary in their effects but sickle cell anaemia, commonly caused by haemoglobin SS and beta-thalassemia major, is known to be particularly detrimental and severely impact patients’ quality of life. One way these conditions are managed is through blood transfusions, as these can replace the patient’s unhealthy red blood cells with healthy ones from a person without sickle cell disease, improving symptoms. Although much effort is put into matching patients with suitable blood donors, the UK’s National Health Service (NHS) estimates that one-fifth of patients will develop antibodies against donated blood due to differences in the characteristics of their blood after transfusion. Finding compatible blood donors is crucial as people with sickle cell disease who require multiple blood donations can suffer from detrimental side effects attributed to donor incompatibility.
Starting 22 January 2024, the NHS has implemented an innovative way to better match patients and blood donors to combat this incompatibility. This new test, stated to be the world’s first “blood matching” test, aims to look at people’s genes to find donors that suit them best. As a person’s genes are highly specific, this test will match patients with donors who are compatible with their unique needs, minimising the chances of side effects or antibody development. Additionally, as the test is provided through the NHS, it will be freely available for those with sickle cell disease, making it instrumental in reducing health inequalities.
Although blood transfusion for sickle cell disease is not a cure, this novel blood-matching test can improve its effectiveness as a treatment. Those with subtypes that cause sickle cell anaemia and require blood transfusions, haemoglobin SS and beta-thalassemia major, are particularly likely to benefit. This is especially significant as GlobalData epidemiologists forecast that the number of prevalent cases of these subtypes will rise in the UK, although the prevalence rate will remain the same. GlobalData epidemiologists estimate the number of diagnosed prevalent cases of hemoglobin SS (HbSS), for all ages in the UK will increase from 12,400 cases in 2024 to 12,700 in 2030. Additionally, the number of diagnosed prevalent cases of beta-thalassemia major (HbSß0 tha) for all ages in the UK is expected to increase from 815 cases in 2024 to 850 in 2030.