As the stigma surrounding mental health continues to diminish, health professionals have begun to shed light on the risk of suicide. Among the populations considered in this trend are individuals with terminal illnesses, who are the focus of a recent publication in The Lancet, by Nafilyan and colleagues. This population-based study, which explored the relationship between terminal illness diagnosis dates and patient suicide rates in England, revealed that individuals diagnosed with conditions with a high risk of death faced an increased risk of suicide. Moreover, the hazard risk of suicide was highest across all cohorts within a year of diagnosis or initial treatment. GlobalData epidemiologists forecast a rise in the prevalence of several of the diseases observed in the study across the 16MM (the US, France, Germany, Italy, Spain, the UK, Japan, Australia, Brazil, Canada, China, India, Mexico, Russia, South Africa, and South Korea), underscoring the need for a comprehensive understanding of terminal disease patients’ mental health.
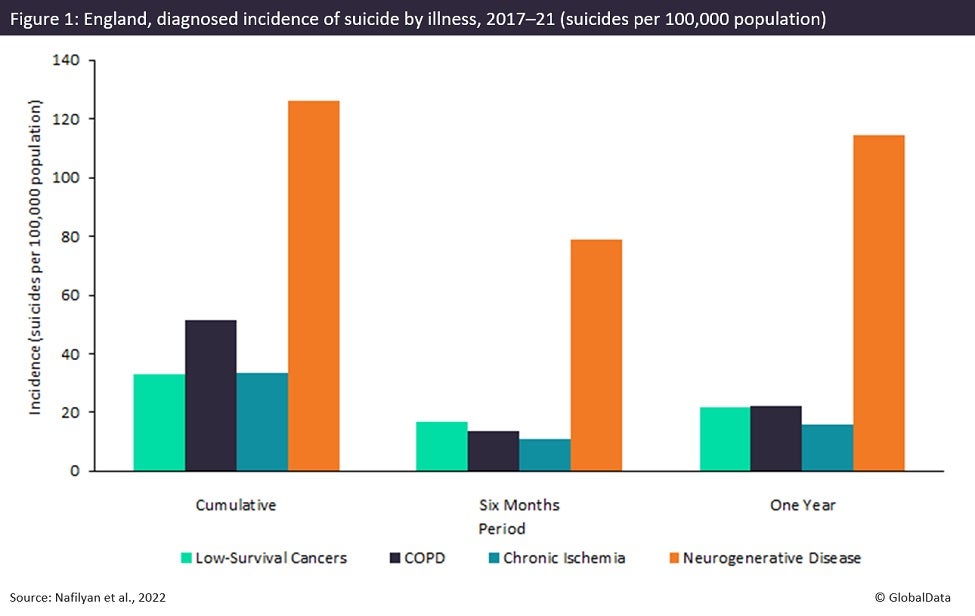
Nafilyan and colleagues conducted a retrospective cohort study using the Hospital Episode Statistics (HES) entries and death registration records for 47,354,696 individuals between 2017–2021. Deaths caused by intentional self-harm were linked to health records showing first diagnoses of low-survival cancers, chronic obstructive pulmonary disease (COPD), degenerative neurological diseases (i.e., Huntington’s and motor neuron diseases), and chronic ischemic heart disease. The entire study population, including those without terminal illnesses, showed a suicide incidence rate (defined as suicides per 100,000 population) of 36.3. While individuals with a low-survival cancer or chronic ischemic heart disease diagnosis showed a slightly lower incidence of suicide at 32.8 and 33.6, respectively. Conversely, the suicide incidence was 51.4 among those diagnosed with COPD and 126.0 among those diagnosed with degenerative neurological conditions. Furthermore, the rate of suicide in these groups was particularly high in the first few months following diagnosis. For example, the rate of suicide six months following diagnosis was 16.6 among low-survival cancer patient compared to 5.7 in the control group. This rate rose to 21.6 one year after diagnosis compared to 9.5 in the control group. Throughout the study period, the hazard rate of death due to suicide was higher among all groups diagnosed with a terminal illness than their matched controls, with a spike in the first months followed by a stabilizing but elevated rate thereafter.
The results of Nafilyan and colleagues’ study sheds a light on severe mental health toll exacted upon patients with terminal diseases. GlobalData epidemiologists project that the diagnosed prevalent cases of several terminal illnesses are expected to rise over the next decade. Diagnosed prevalent cases of COPD are expected to grow from almost 115.1 million to approximately 141.5 million between 2018 and 2028 in the 16MM. Similarly, there is an expected rise in the diagnosed prevalent cases of Huntington’s disease, exceeding 125,000 in 2020 and increasing to over 135,000 cases in 2030 across the 16MM. The growing burden of terminal diseases necessitates counseling and support networks for affected patients. Furthermore, Nafilyan and colleagues’ work emphasizes the importance of intensive monitoring for signs of suicidal ideation in the earliest months of diagnosis.