Travere Therapeutics’ sparsentan could replace first-line (1L) standard-of-care (SOC) treatment in newly diagnosed focal segmental glomerulosclerosis (FSGS), some experts said. However, others noted an attempt at remission with current care should be tried first, or sparsentan should at least be attempted in tandem. Ultimately, a personalised treatment approach might be the best option.
In addition to angiotensin-converting enzyme (ACE) inhibitors/angiotensin-receptor blockers (ARBs), immunosuppressive therapies including steroids are considered part of 1L SOC treatments in FSGS, but there are no FDA-approved therapies. If sparsentan reduces proteinuria in comparison to generic ARB irbesartan in the Phase III DUPLEX study, some experts said it would be sufficient evidence to supplant the drug class in the frontline setting.
However, experts had mixed views on its use regarding immunosuppressive drugs either in combination with steroids or after steroids have failed to induce remission. Factors such as disease variability among patients and individual physician preferences will likely play roles in deciding sparsentan’s position in the treatment sequence for FSGS. While those with poorly controlled proteinuria could benefit from sparsentan’s dual action, considering the differences in FSGS’ clinical manifestation, further proteinuria reduction among stable patients would need to be assessed on an individual basis, said experts.
Travere, previously known as Retrophin, plans to release topline efficacy data on the 36-week proteinuria endpoint in DUPLEX in February, as per an 11 January update. The company plans to file for an FDA accelerated approval and a conditional marketing authorisation in Europe based on DUPLEX results in 2H21.
DUPLEX has two coprimary endpoints of proteinuria reduction and slope of estimated glomerular filtration rate (eGFR). While the former is considered a surrogate marker, experts found it a fair assessment of FSGS outcomes. An accelerated approval is probable, they said, following potentially positive Phase III results.
One analyst estimated peak sales of $2.1bn in FSGS with a 75% probability of success. Travere’s market cap is $1.39bn. A second analyst was also reasonably optimistic about the trial’s success based on Phase II DUET results and the DUPLEX design, but did not elaborate on what trial features are favourable. Travere declined to comment on this story, citing the upcoming results.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataSparsentan use in treatment paradigm debated
The goal of treatment is to reduce proteinuria as quickly as possible, so there would be an impetus to put patients on sparsentan immediately after diagnosis, said a European nephrologist. Some genetic subtypes of FSGS may not benefit from immunosuppressive therapies, and drugs like sparsentan could be useful as 1L therapies, said Dr Michelle Rheault, director, Division of Paediatric Nephrology, University of Minnesota Medical School, Minneapolis. Complete remission rates following initial immunosuppressive treatment is 32–47% (Korbet et al.; JASN November 2012, 23 (11) 1769–1776).
In DUPLEX, patients on immunosuppressive drugs like Roche and Biogen’s Rituxan (rituximab), Bristol-Myers Squibb’s Orencia (abatacept) or cyclophosphamide within three months of screening were excluded, but those on other immunosuppressive therapies were allowed if the dosage was stable prior to screening.
Nonetheless, sparsentan’s 1L use may not be automatic. Very few patients stay in remission following immunosuppressive drugs, but it would be preferable to try these therapies first in case they can go into complete remission before putting them on a chronic treatment with another new drug, said Dr Pascale Lane, section chief, Section of Nephrology, University of Oklahoma Health Sciences Centre, Oklahoma City. However, since there are no added toxicities with combining sparsentan and corticosteroids, there is no reason to wait to start the one drug only after the other fails, the European nephrologist said.
Responses within primary FSGS are variable, so while some patients progress very rapidly, others have a slowly progressive disease, Lane said. As such, a personalised treatment approach is important because FSGS is not a uniform disease, and even two patients who have identical clinical characteristics may not respond the same way to a therapy, she said. Moreover, since patients are on several different immunosuppressive regimens, it would be difficult to identify signals from each subgroup of DUPLEX to guide treatment decisions, said Rheault.
The drug will likely initially be used as an add-on or rescue therapy, and biomarkers can help identify patients who may respond well to it in the frontline setting, Rheault said. Sparsentan has dual action of blocking endothelin type A receptor and angiotensin II receptor, while its comparator in DUPLEX— irbesartan—blocks angiotensin II receptor.
In terms of those competing with standard ARBs, physicians will likely switch patients if sparsentan proves superior to its competitor, said a US-based nephrologist. However, individual clinical judgement would be necessary to determine whether further proteinuria reduction is required, noted the US-based nephrologist and Lane. The European nephrologist elucidated this with an example of switching to sparsentan if patients are still proteinuric on current treatments. In FSGS, 70% of adults present with proteinuria, which is in the nephrotic range or more than >3g of protein/d. But for patients with low-grade proteinuria, classified as less than 1–2g protein/d, there would be no indication to change their existing treatment, he added. Payers are unlikely to put pressure to switch someone who is doing well on their current therapy, said Lane.
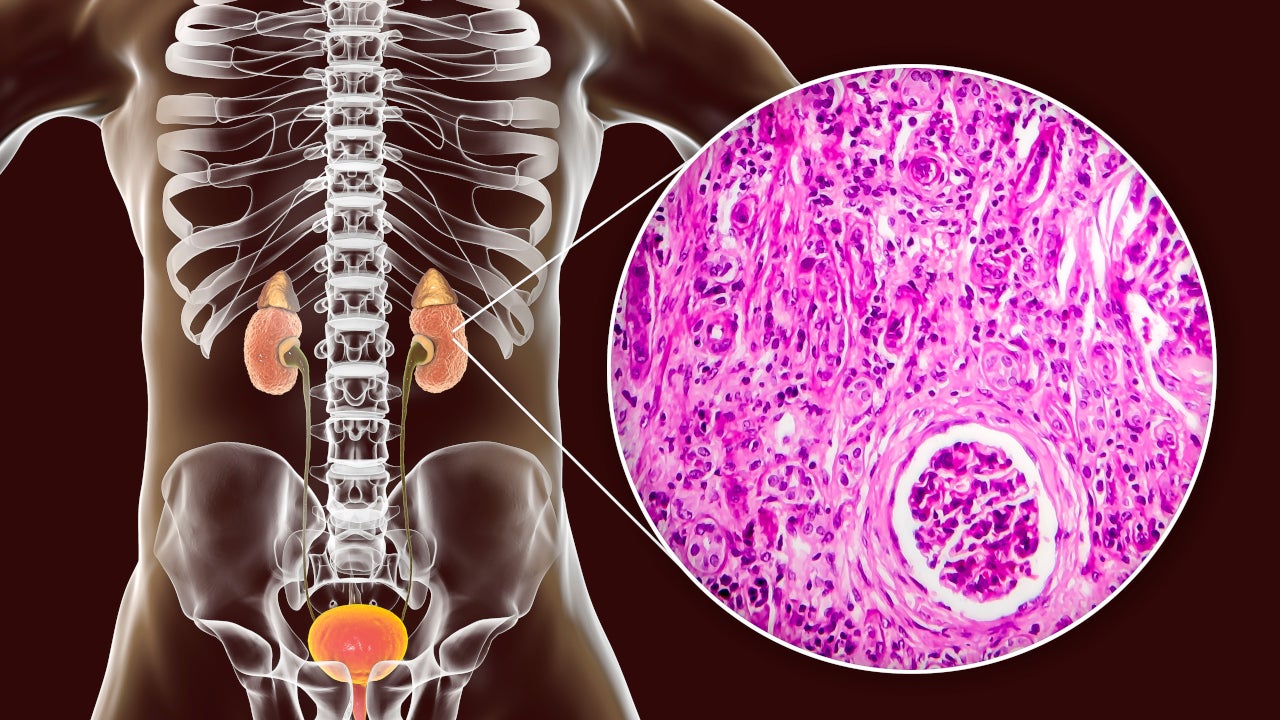
FSGS is classified as a rare disorder, with approximately 5,400 patients diagnosed each year, and an estimated 19,306 patients living with end-stage kidney disease due to FSGS, according to the non-profit organisation Nephcure.
While sparsentan has the lead on potentially being the first FDA- approved therapy for FSGS, others with a more distinct mechanism may soon pose competition. Experts referred to targeted approaches like Cambridge, Massachusetts-based Goldfinch Bio’s TRPC5 inhibitor GFB-887, which is undergoing studies with biomarkers being used to predict the patients who will have a favourable response to a drug. A Phase II study is evaluating GFB-887 in different kidney disorders, including FSGS, specifically in patients with overactivation of the TRPC5-Rac1 pathway.
Regulatory expectations for sparsentan
The DUET study results on proteinuria reduction were significant, and DUPLEX results should reflect the earlier data, said the European nephrologist. In the DUET trial, sparsentan-treated patients had 45% reductions in urine protein-to-creatinine ratio (UP/C) versus irbesartan-treated patients when different dose cohorts were pooled for analysis (Trachtman et al.; J Am Soc Nephrol; 2018 Nov;29(11):2745–2754). A 45% proteinuria reduction is an advance in the field, said Lane, but she and the US nephrologist declined to comment on upcoming DUPLEX results.
Apart from the addition of the coprimary endpoint of slope of estimated glomerular filtration rate (eGFR) from week 6 to week 108 in DUPLEX, proteinuria reduction will be measured at 36 weeks as opposed to eight weeks in DUET.
Based on the open-label extension of the DUET study, the proteinuria reduction is sustained on whether sparsentan efficacy can be seen in longer-term studies like DUPLEX, said the US nephrologist. Among 45 patients who received sparsentan, median UP/C was reduced from 2.8g/g at baseline to 0.9g/g at week 84, as per a 26 October 2018 press release. Moreover, 26 patients in the control arm who crossed over to sparsentan experienced median UP/C decreasing from 2.3g/g at crossover (week eight) to 1.1g/g at week 84, according to the same release.
Nevertheless, while reducing proteinuria can make patients feel better, it is not universally appreciated to judge drug efficacy for full regulatory approvals, said Lane. DUPLEX is supposed to prove whether proteinuria reduction is associated with hard clinical outcomes, said the US nephrologist. However, the accelerated approval would be driven by the proteinuria reduction, which experts considered a good surrogate in glomerular disorders like FSGS, pending confirmatory eGFR data. The long-term kidney function data, measured by the slope of eGFR, will ultimately be the gold standard to judge both the drug’s efficacy and whether sparsentan’s dual action is more potent than ARBs alone, said Lane. It would be important to show a trend in eGFR changes as well, said the European nephrologist.
In DUET, side effects like hypotension and edema were observed, as per the data abstract. Observed side effects due to low blood pressure in DUET showed the importance of titrating sparsentan doses, said the European nephrologist. However, titrating drugs and managing side effects like edema is standard in nephrology, he said, noting he did not anticipate any major challenges with its use.
Manasi Vaidya is a Senior Reporter for Clinical Trials Arena parent company GlobalData’s investigative journalism team. A version of this article originally appeared on the Insights module of GlobalData’s Pharmaceutical Intelligence Center. To access more articles like this, visit GlobalData.