On 11 June 2009 the H1N1 strain of influenza A officially became a global pandemic. Since then, pharmaceutical companies have ramped up vaccine production and the first known fatality outside the Americas has been reported in the UK. The threat, it seems, is slowly gaining force.
As the World Health Organization (WHO) raised its alert over the 2009 influenza outbreak to Level Six, more than 30,000 were suffering from the illness around the world. WHO director general Dr Margaret Chan confirmed that the virus is still contagious and is spreading easily from one person to another. A total of 74 nations have been affected.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
With its new pandemic status, the WHO has given this strain the most serious outlook awarded to any outbreak of influenza in 41 years. More than 1,400 cases have been officially confirmed in Australia and the death toll has hit six in Canada. In addition, around three quarters of the victims are under the age of 30.
But Chan is confident it is not all doom and gloom. Artificial strains that will form the basis of vaccines have been delivered to pharmaceutical companies for them to create a vaccine and stocks of anti-viral treatments such as Tamiflu are still in ready supply.
The danger remains, however, that the treatments will not match an even more severe strain that could rear its head if the virus mutates further. Much of this year’s seasonal flu strain has developed Tamiflu resistance, according to some experts, and there is no reason why H1N1 won’t either.
Responses to the crisis around the world have been on the one hand coordinated – with border agencies and health departments working together – and on the other incredibly varied in their response.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataFor example, in Jordan officials have announced that 80% of the population will receive the vaccine once it has been produced.
Meanwhile, in the UK National Health Service (NHS) doctors are threatening to walk out, fearing they will be sued over the care they will be able to provide if infections become more widespread, according to a BBC report.
Around the world pharmaceutical companies large and small are united in doing their best to produce a vaccine and cash in on a billion-dollar pandemic.
The race is on
On 15 June 2009 GlaxoSmithKline (GSK) responded to the pandemic announcement by stating that it was increasing the production and supply of its anti-viral medication Relenza, as well as focusing efforts on an adjuvant vaccine.
GSK received the seed strain from the WHO at the end of May 2009 and is developing the new vaccine at its Canadian and German manufacturing sites. The first doses of the antigen are expected sometime between September and November, if all goes well with the regulators.
The company has also committed to donating 50 million doses of the vaccine and as capacity increases, will offer less economically developed countries the drug on a tiered-pricing policy based on World Bank classifications.
Splitting the industry is the decision by Novartis to go against this trend, as it announced it was ruling out donating any vaccines to low-income nations.
Novartis chief executive Daniel Vasella told the Financial Times that although the company may offer discounts, giving away the drugs for free was not an option. “If you want to make production sustainable, you have to create financial incentives,” he said.
On 15 June Novartis announced that it had successfully completed production of the first batch of the vaccine, weeks ahead of schedule. The 10l batch “will be used for pre-clinical evaluation and testing, and is also being considered for use in clinical trials”, the company said.
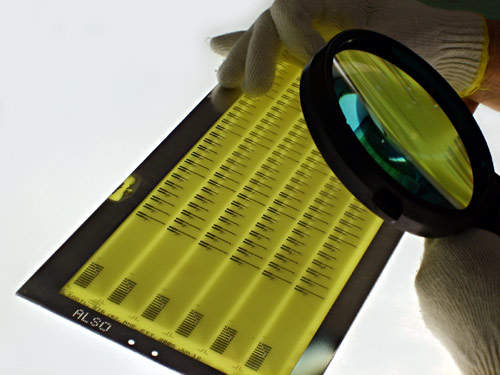
More than 30 countries have put in orders for the vaccine’s ingredients and Novartis is hoping to be first to market by using cell culture-based technology rather than growing the vaccine in eggs. Although the majority of firms will use hen eggs for vaccine production the method carries risks as the eggs can be susceptible to infections. The quantity of virus particles that will be produced is as yet unknown.
Another firm opting for cell technology is Baxter International, in full-scale production of its proprietary CELVAPAN brand after completing testing and evaluation.
A number of national public health authorities have existing pandemic agreements with Baxter that allow them to place orders for a vaccine now that a pandemic has been declared.
These are just a few of the firms in the race and most hope to release their versions by the third quarter of 2009. But despite assurances from the WHO that this strain has been identified early on, it is hard not to draw comparisons with the 1918, 1957 and 1968 outbreaks which claimed the lives of millions.
As the disease spreads it also constantly mutates and it is this degree of uncertainty that adds an extra element of risk.
If the disease continues to spread and reaches areas previously infected by the highly virulent bird flu, the situation could yet be disastrous.





