Humira (adalimumab) is a monoclonal antibody indicated for the treatment of more than ten indications, including rheumatoid arthritis (RA), juvenile idiopathic arthritis (JIA), psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, plaque psoriasis, hidradenitis suppurativa (HS), and uveitis.
The drug was originally developed by Abbott and is currently marketed by its spin-off AbbVie. It was first approved by the US Food and Drug Administration (FDA) for the treatment of rheumatoid arthritis in 2002. AbbVie and Eisai co-market Humira in Japan.
The European Medicines Agency (EMA) approved the drug for RA in 2003, followed by the Pharmaceuticals and Medicals Devices Agency of Japan (PMDA) in 2008, and China Food and Drug Administration (CFDA) in 2010. Over the years, Humira has received label expansion for several other autoimmune diseases from the regulatory bodies.
Humira became the first approved drug for the treatment of hidradenitis suppurativa worldwide after recieving approval in Japan in February 2019. It also received approval for HS treatment in the US and Europe in 2015. Humira further holds the FDA’s orphan drug designation for moderate to severe HS treatment.
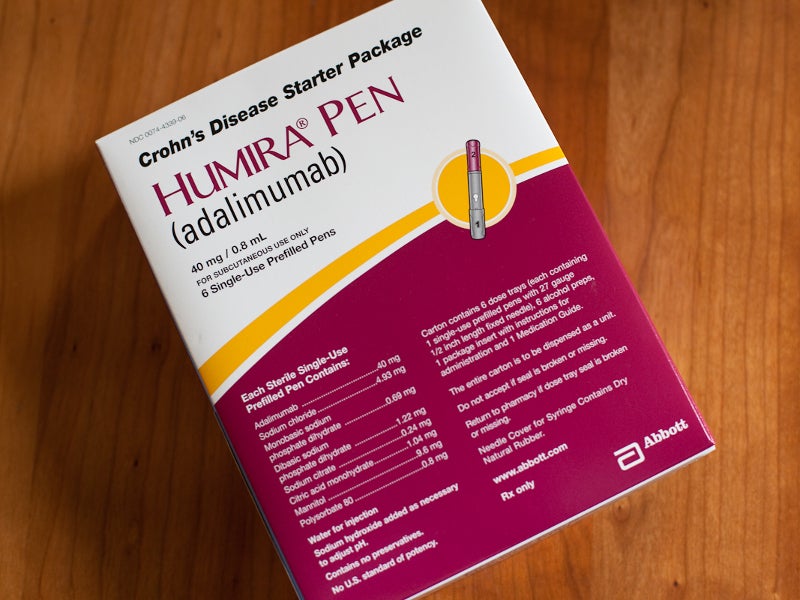
The drug is available as a sterile solution for subcutaneous administration in various dosage forms such as single-use Humira pen, prefilled glass syringe, and glass vials.
Hidradenitis suppurativa causes and symptoms
HS is a chronic, debilitating, inflammatory skin disorder, which causes painful lesions on various parts of the body such as armpit, breasts and groin. It progresses into abscesses and fistulas, causing pus discharge.
Development of swollen, red-coloured nodules and abscesses are the common symptoms of the disease. The condition impacts less than 1% of the adult population worldwide.
Humira’s mechanism of action
Humira is an alpha tumour necrosis factor (TNF) inhibitor, which specifically binds to TNF-alpha and blocks its interaction with p55 and p75 TNF receptors on the cell surface.
TNF is a cell signalling protein found in the body that is responsible for natural inflammatory and immune responses. Increased level of TNF in the body leads to various autoimmune diseases such as arthritis, psoriasis, and ankylosing spondylitis. Humira alters the biological reactions occurring due to TNF.
Clinical studies on Humira for HS
Japanese approval of the drug was based on a phase three multi-centre, open-label, single-arm study on 15 Japanese patients with moderate to severe HS, as well as two overseas phase three randomised, double-blind, placebo-controlled studies named Pioneer I and II, which enrolled 633 patients.
Hidradenitis Suppurativa Clinical Response (HiSCR) at week 12 was the primary endpoint in all the studies. HiSCR is the measure to determine at least a 50% reduction in inflamed nodule count or pus discharge.
The patients received a 160mg dose of either Humira or placebo at week zero, an 80mg dose at week two, and a 40mg dose at week four, which was continued until week 11.
In the Japanese study, 13 out of 15 patients achieved the primary endpoint at week 12. The most common adverse events observed in the patients at week 24 were adverse drug reactions.
In Pioneer I, patients receiving Humira demonstrated 64% HiSCR compared to 26% HiSCR in patients receiving a placebo. In Pioneer II, 59% HiSCR was observed in patients receiving Humira, compared to 28% HiSCR in those on placebo.
The most adverse events reported in the patients in the Pioneer studies were injection site reactions, headache, rash and infections, particularly upper respiratory and sinusitis.