Lynparza® (olaparib) is a targeted therapy indicated for the treatment of adults with advanced ovarian cancer, deleterious or suspected deleterious germline BRCA mutated (gBRCAm) HER2-negative high-risk early breast cancer, pancreatic cancer and prostate cancer.
The drug is being developed by AstraZeneca, a UK-based biopharmaceutical company, in collaboration with Merck & Co, a pharmaceutical company based in the US, under a strategic oncology collaboration agreement signed in July 2017. It is being developed in combination with the companies’ PD-L1 and PD-1 inhibitors as part of their collaborative efforts.
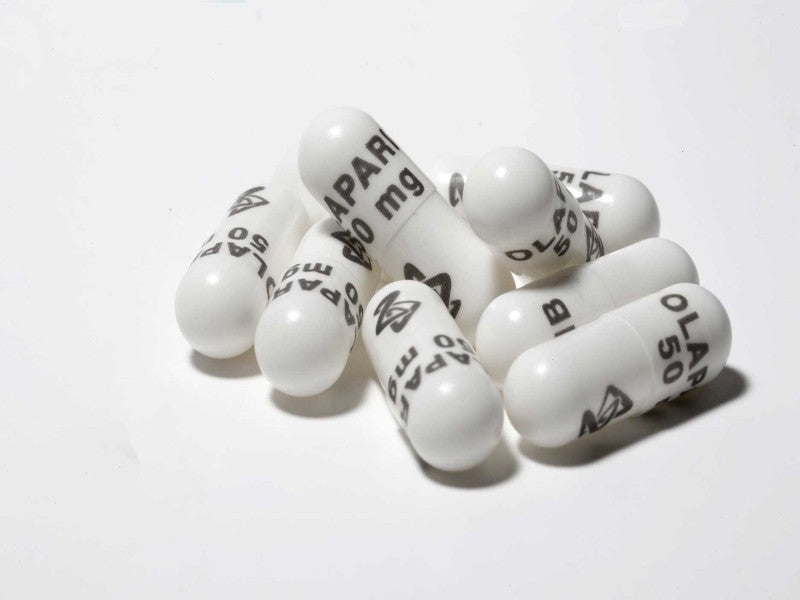
The drug is available as oval, biconvex, film-coated tablets in green to green/grey 150mg and yellow to dark yellow100mg dosage strengths. It is also available as 50mg white, opaque capsules marked in black ink with “OLAPARIB 50 mg” on the cap and the AstraZeneca logo on the body.
Regulatory approvals of Lynparza
Lynparza received its first regulatory approval from the European Medicines Agency (EMA) for the treatment of advanced ovarian cancer associated with BRCA mutations in December 2014.
The US Food and Drug Administration (FDA) approved Lynparza 400mg twice-daily capsules in the same month under its accelerated approval programme, as the first treatment for patients with deleterious or suspected detrimental gBRCAm advanced ovarian cancer.
In August 2017, the FDA granted regular approval to Lynparza for the maintenance treatment of recurrent ovarian cancer, based on two randomised, placebo-controlled, double-blind, multi-centre trials in patients with recurrent ovarian cancers who responded to platinum-based therapy.
In January 2018, the FDA approved the drug for the treatment of HER2-negative metastatic breast cancer with gBRCA mutations.
Health Canada authorised Lynparza as monotherapy in May 2018 for the treatment of adult patients with deleterious or suspected deleterious gBRCAm, HER2-negative metastatic breast cancer.
Lynparza was approved by the FDA and China’s National Medical Products Administration (NMPA) in December 2018 and December 2019 respectively, as a maintenance treatment for adult patients with deleterious or suspected deleterious germline or somatic BRCA-mutated (gBRCAm or sBRCAm) advanced epithelial ovarian, fallopian tube or primary peritoneal cancer.
Health Canada approved Lynparza as a maintenance treatment for adult patients with advanced BRCAm high-grade epithelial ovarian, fallopian tube or primary peritoneal cancer in May 2019.
The FDA approval was extended to include the treatment of pancreatic cancer and maintenance therapy for certain prostate cancers in December 2019.
Lynparza in combination with bevacizumab was approved by the FDA for homologous recombination deficiency (HRD)-positive advanced ovarian cancer in May 2020. In the same month, the FDA approved olaparib for adult patients with deleterious or suspected deleterious germline or somatic homologous recombination repair (HRR) gene-mutated metastatic castration-resistant prostate cancer (mCRPC), whose cancer progressed following prior treatment with enzalutamide or abiraterone.
The European Union (EU) authorised Lynparza in November 2020 for patients with mCRPC with breast cancer susceptibility gene 1/2 (BRCA1/2) mutations.
In March 2022, Lynparza was authorised as adjuvant therapy in the US for patients with gBRCAm HER2-negative high-risk early breast cancer.
In August 2022, Lynparza was authorised in Japan by the Ministry of Health, Labour and Welfare (MHLW)as an adjuvant therapy for BRCA-mutated, HER2-negative, high-risk early breast cancer.
Lynparza in combination with abiraterone and prednisone or prednisolone was approved in the EU in December 2022 for the treatment of mCRPC in adult men,
Lynparza in combination with abiraterone and prednisone or prednisolone was authorised by the FDA in May 2023 and by the Japan MHLW in August 2023 for the treatment of adult patients with deleterious or suspected detrimental BRCAm and mCRPC.
BRCA-mutated ovarian and breast cancer
BRCA mutation is a mutation in the either BRCA1 genes or BRCA2 genes. These mutations disable an important DNA repair process and significantly increase the risk of developing ovarian cancer and other cancers.
Breast cancer BRCA1 and BRCA2 genes are most often affected in hereditary breast and ovarian cancer. Inherited mutations in these genes cause around 3% of breast cancers (approximately 7,500 women per year) and 10% of ovarian cancers. Breast or ovarian cancer does not affect everyone who inherits one of these mutations. Cancer develops when a second mutation affects the normal copy of the gene.
Metastatic breast cancer is the most advanced stage of breast cancer (Stage IV) and occurs when cancer cells have moved outside of the breast to other regions of the body. There is presently no treatment for MBC, and only 26.9% of patients survive five years following diagnosis.
Pancreatic cancer
Pancreatic cancer is the seventh leading cause of cancer death globally. As there are often no symptoms or symptoms that are non-specific in the early stages, it is most diagnosed at an incurable stage.
Around 80% of patients are diagnosed when the disease has metastasised and for these, the average survival is less than a year. Current treatment is surgery, chemotherapy and radiotherapy, highlighting a critical unmet medical need for more effective treatment options.
Lynparza’s mechanism of action
Lynparza contains an active component called olaparib, which is a poly ADP ribose polymerase (PARP) inhibitor. It exploits tumour DNA repair pathway deficiencies and kills cancer cells. The mechanism of action gives the drug the potential to fight against a range of tumours with DNA repair deficiencies.
Clinical trials on Lynparza
The FDA approval for Lynparza is based on results from a Phase II clinical trial conducted on patients with deleterious or suspected deleterious gBRCAm advanced cancers to determine the safety and efficacy of the drug.
The single-arm, open-label study enrolled 137 gBRCAm ovarian cancer patients who had received three or more prior lines of chemotherapy.
The study met all its primary endpoints with a response rate of 34%. The median response duration was 7.9 months. The common adverse reactions recorded were nausea, vomiting, anaemia and fatigue.
The SOLO programme includes three individual Phase III clinical trials known as SOLO1, SOLO2 and SOLO3.
SOLO1 evaluates olaparib as a maintenance monotherapy for ovarian cancer patients who were completely or partially responsive to first-line platinum-based chemotherapy.
SOLO2 evaluates olaparib as a maintenance monotherapy for relapsed ovarian cancer patients who were completely or partially responsive to first-line platinum-based chemotherapy. The study supported the full approval of the drug for recurrent ovarian cancer.
SOLO3 compares olaparib with non-platinum chemotherapy as third-line or later treatment for relapsed ovarian cancer patients.
Both SOLO-1 and SOLO-2 trials demonstrated significant improvements in progression-free survival (PFS) with Lynparza compared to placebo. Lynparza reduced the risk of disease progression or death by 70% in both newly diagnosed and relapsed BRCAm ovarian cancer patients.
Additional clinical trials on Lynparza
The approval of Lynparza (olaparib) for the treatment of gBRCAm, HER2-negative metastatic breast cancer was based on data from the open-label, multi-centre, randomised trial OlympiAD, enrolling 302 patients with germline BRCA-mutated, HER2-negative metastatic breast cancer.
Patients were randomised in a 2:1 ratio. A total of 205 patients received olaparib tablets, 300mg orally twice daily, and 97 patients received the physician’s choice of chemotherapy, which included capecitabine, vinorelbine or eribulin.
The olaparib group met the primary endpoint with a median PFS of seven months compared to 4.2 months in the chemotherapy group.
The POLO trial was a pivotal Phase III, double-blind, placebo-controlled, multi-centre clinical trial aimed at investigating the efficacy of Lynparza in patients with gBRCAm metastatic pancreatic adenocarcinoma.
The study randomised (3:2) 154 patients with gBRCAm metastatic pancreatic adenocarcinoma to 300mg twice daily olaparib or placebo until disease progression or unacceptable toxicity.
The main efficacy outcome measure was PFS. Median PFS was 7.4 months for patients who received olaparib compared with 3.8 months for patients who received placebo.
The efficacy of the drug for HRR gene-mutated mCRPC was evaluated in PROfound, an open-label, multi-centre trial, randomising (2:1) 256 patients to 300mg twice daily olaparib and 131 patients to investigator’s choice of enzalutamide or abiraterone acetate. Radiological progression-free survival (rPFS) was the primary endpoint. The drug showed a statistically significant improvement in rPFS compared to the control group.
The Phase III PROpel trial supported the FDA’s approval of Lynparza in combination with abiraterone and prednisone or prednisolone for the treatment of adult patients with BRCA-mutated mCRPC. The trial showed that the combination reduced the risk of progression or death by 34% compared with abiraterone alone. It also significantly improved rPFS over placebo and abiraterone alone. The median rPFS was 24.8 months with the combination, compared with 16.6 months with abiraterone alone. The Lynparzacombination reduced the risk of disease progression or death by 76% compared to abiraterone alone.