Paxil (paroxetine hydrochloride) was first developed in 1975 by a Danish company called Ferrosan. During 1980 Ferrosan sold paroxetine to Beecham Pharmaceuticals which later merged with SmithKline & French to become SmithKline Beecham. During 2000 the company merged with Glaxo to form GlaxoSmithKline (GSK)
Paxil is indicated for the treatment of a range of conditions which are known as major depressive disorders (MDD). These conditions include post-traumatic stress disorder, panic disorder, social anxiety disorder and obsessive compulsive disorder. In adults the efficacy of paroxetine for depression is comparable to that of older tricyclic antidepressants, with fewer side effects and lower toxicity.
The effectiveness of paroxetine in the treatment of MDD was proven by six placebo-controlled clinical trials.
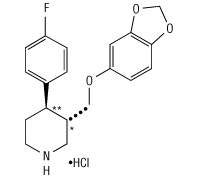
Paroxetine – clinical pharmacology
Paroxetine is a selective serotonin reuptake inhibitor (SSRI) antidepressant that was first marketed in 1992.
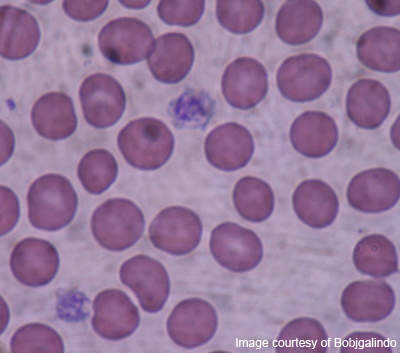
Studies at clinically relevant doses in humans have demonstrated that paroxetine blocks the uptake of serotonin into human platelets. In vitro studies also suggest that paroxetine is a potent and highly selective inhibitor of neuronal serotonin reuptake and has only very weak effects on norepinephrine and dopamine neuronal reuptake.
Approvals
Since its launch paroxetine has been approved for a number of conditions.
During 1996 it was approved for treatment of major panic disorder and obsessive compulsive disorder. It is said that major panic disorder will affect three to six million US citizens in their lives. Clinical results showed that in one ten-week-double blind study 76% of subjects treated with 40mg/day of Paxil were completely free of full panic attacks at the end point compared with 44% of subjects who received a placebo.
During 1999 the US Food and Drug Administration (FDA) approved Paxil for the treatment of social anxiety disorder, also known as social phobia, affecting more than 10 million US citizens. Results from three multi-centre, placebo-controlled trials of adults demonstrated that Paxil was significantly more effective than the placebo in treating social anxiety disorder.
During 2000 SmithKline Beecham submitted a Supplemental New Drug Application to the FDA for Paxil, seeking marketing approval of Paxil for the treatment of post-traumatic stress disorder (PSTD). Approval was subsequently granted.
Data from a clinical programme involving nearly 1,200 patients diagnosed with PTSD demonstrated the benefit of Paxil over a placebo in reducing PTSD symptoms as measured by the Clinician Administered PTSD Scale and the Clinical Global Impressions Scale, both established standards.
During 2001 the FDA approved Paxil for the treatment of generalised anxiety disorder. The condition is characterised by excessive anxiety and worry about a number of event or activities. According to GSK, the disorder affects more than 60 million Americans.
Post-marketing reports and warnings
Information from the FDA indicates that there have been a number of voluntary reports of adverse events in patients taking Paxil since market introduction. The events, which may have no relationship with the use of the drug, include acute pancreatitis, toxic epidermal necrolysis, acute renal failure, pulmonary hypertension, anaphylaxis and eclampsia.
During April 2004 the European Medicines Agency (EMEA) completed an EU-wide review for paroxetine-containing medicines. The review was initiated in the UK in 2003 on the basis of safety concerns relating to the potential risk of emotional changes (such as mood fluctuations, hostility, self harm, suicidal thoughts and attempted suicide) and withdrawal reactions associated with the use of paroxetine.
The committee concluded that the benefit-risk level remained positive for the products but recommended that paroxetine should not be given to children and adolescents as clinical trials indicated that its use was associated with increased risk of suicidal behaviour and hostility.
The EMEA also recommended the close monitoring of adult patients at high risk of suicidal behaviour or thoughts and that those wishing to terminate the use of paroxetine should reduce its use gradually, because of reports of adverse withdrawal reactions.
During 2005 the FDA issued an alert to healthcare professionals and patients about early results of studies, which indicated that paroxetine increased the risk of birth defects, particularly heart defects when women took the drug during the first three months of pregnancy. The FDA advised healthcare professionals not to prescribe Paxil to women who were in the first three months of pregnancy or were planning pregnancy unless other treatment options were not appropriate.
In light of the findings the FDA asked GSK to change the pregnancy category of Paxil from C to D, a stronger warning. Category D means that studies in pregnant women (controlled or observational) had demonstrated a risk to the foetus. However, the benefits of the therapy may outweigh the potential risks to the foetus.
An FDA alert issued in 2006 also indicated that there was an increased risk of neonatal persistent pulmonary hypertension in infants born to mothers who took SSRIs after the 20th week of pregnancy. A number of SSRIs, including Paxil, were listed by the FDA.
Further studies led GSK, during 2006, to notify healthcare professionals about new warnings on the risk of suicidal tendencies for adult patients, especially young adults aged 18 to 24.
GSK said that it had completed a meta-analysis of clinical trials in adult patients with MDD taking paroxetine. The analysis looked at suicidal behaviour and ideation and showed a higher overall frequency – two in 100 vs one in 100 – of suicidal behaviour in adults aged 18 to 24 treated with Paxil compared with a placebo. This was not observed in older adults.
For adults with MDD the frequency of suicidal behaviour was higher for patients of all ages treated with paroxetine compared with a placebo – about 30 in 10,000 compared with five in 10,000. However, the majority of suicide attempts in these patients were in those aged 18 to 30. This suggested that the higher frequency of suicidal tendencies seen in younger patients across psychiatric disorders may extend beyond the age of 24.
As a result of the findings, GSK said that it was important for all patients, especially young adults, to be carefully monitored during paroxetine therapy regardless of the condition being treated.