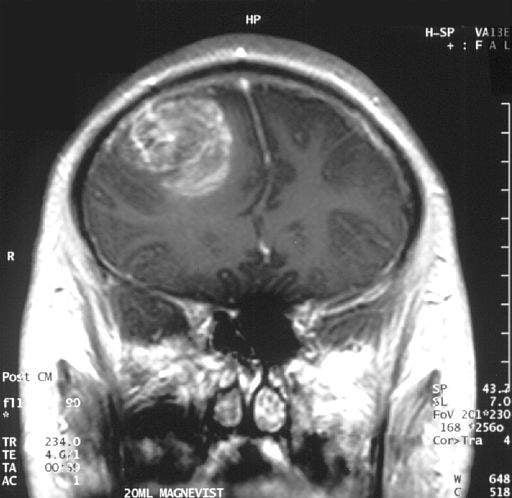
Scientists at the Salk Institute have generated aggressive glioblastoma multiforme (GBM) tumours in an attempt to discern tumour activity and progression, and investigate new cancer drugs and personalised treatments.
The researchers grew the tumours in a dish by editing two genes in human cerebral organoids. The study was published on 24 April in the journal Cell Reports.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
GBM, a form of brain cancer, has previously proven elusive due to the difficulty in observing the tumours’ progression in their natural environment. The recent study provides a model which has the potential to offer new insight into this underexplored area.
An additional obstacle to discerning GBM activity is the insufficient data provided by animal models. Differences between animal and human models prove a common problem for clinical trials, with numerous drugs showing promise in animals yet failing in people.
Previously, researchers have used xenografts in their attempts to counter this issue, implanting patient tumour tissue in animal models. However, this approach brings its own problems as sometimes there is not enough human tumour tissue to study, and over time tumours adapt to their new environment.
“As tumours grow in mice, the environment changes the tumour’s features,” the study’s first author Junko Ogawa said. “We don’t know if it’s similar to the patient’s original cancer.”

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataHuman cerebral organoids, which contain neurons and other brain cells, provide a viable alternative. Researchers at the Salk lab used stem cells to create these 3D structures measuring around 4mm, which they hoped to apply in the study of GBM.
Using a CRISPR-Cas9 tool, the team modified HRas and p53, two genes with close links to cancer, into a small number of cells in an organoid. HRas is a cancer oncogene which stimulates cell growth, while p53 works as a tumour suppressor. When edited, these genes turned into tumour-like structures and grew rapidly, demonstrating several similar biomarkers to GBM. Eventually, they overtook the original organoid cells, replacing them with tumour tissue.
Researchers then successfully transplanted them into animal models, where their activity was similarly aggressive.
“You can phenocopy the properties of the tumours in a mouse,” Ogawa said. “Now we can give them drugs to see if they are effective. We can also test the tumour’s ability to invade normal brain tissue.”
A fluorescent red marker known as tdTomato was added to HRas, allowing researchers to track the cell’s progression as it took over the organoids.
This method better mimics the actual development of GBMs in people, as they begin as a small number of aberrant cells rather than a vast number, such as those seen in a xenograft.
The organoids can host human tumour samples and some GBM cell lines, offering a model on which personalised treatments can be tested as patients’ own cancer cells could be transplanted to make the organoid model. This method could be applied to a range of cancer types, not just GBM.





