Contraception is a cornerstone of reproductive health and family planning. Across different markets and cultures, the utilisation and prevalence of female contraception exhibit striking diversity, reflecting the dynamic interplay of social, economic, cultural and healthcare factors. By understanding the determinants that contribute to variation in the prevalence of female contraception, we can gain valuable insight into the broader landscape of women’s health and target interventions and strategies to promote reproductive health.
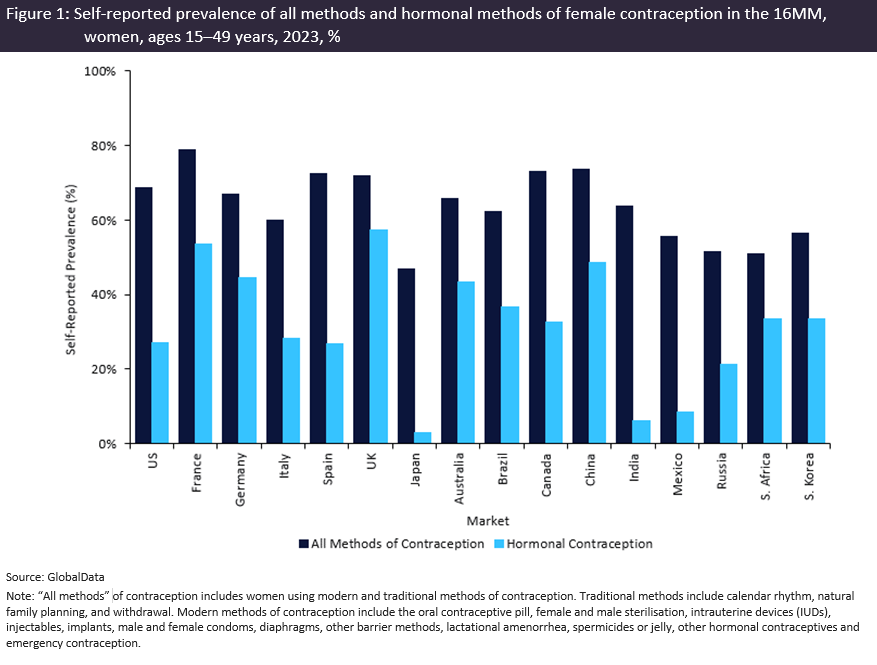
Epidemiology trends from GlobalData’s Epidemiology and Market Size Database show that the prevalence of female contraception, in particular hormonal contraception, varies globally. In 2023, GlobalData calculated that approximately 66% of women ages 15 to 49 years were using at least one method of contraception (as defined in Figure 1 above), and 27% used hormonal contraception, in the 16 major markets (16MM: US, France, Germany, Italy, Spain, UK, Japan, Australia, Brazil, Canada, China, India, Mexico, Russia, South Africa, South Korea) combined. However, when looking at the prevalence of hormonal contraception among individual markets, Japan, Mexico and India emerge as outliers, with prevalence in each market below 10%. Several factors contribute to this trend.
In Japan, the lower prevalence of hormonal contraception in the past decades is because low-dose oral contraceptive pills (one of the most popular methods of female contraception in other industrialised markets) were not legalised until 1999. The most accessible reversible methods of contraception were therefore barrier methods such as male condoms. Concerns about potential side effects or health risks associated with hormonal contraception contribute to the current low prevalence. Currently, oral contraceptive pills require a prescription but are not covered by health insurance. The monthly cost of hormonal contraception may therefore deter women from using it. Additionally, women in rural areas with limited access to health facilities may find it difficult to obtain a prescription.
In Mexico, reasons for the lower prevalence of hormonal contraception may be related to cultural and religious beliefs, preference for tubal ligation as contraception, and limited access to other methods. Although methods such as the oral contraceptive pill are available over the counter, unmarried women experience stigma when trying to access them. Economic status and location also play a role in the choice of contraception. For example, rural patients may have fewer choices of methods available due to shortages in stock.
In India, the lower prevalence of hormonal contraception is in part driven by tubal ligation (a non-hormonal method) being the most extensively used method of contraception. In the past, India has implemented policies and programmes that have emphasised female sterilisation as a means of controlling population growth. While the focus has shifted toward promoting a wider range of contraceptive options, historical policies and incentives may have contributed to the popularity of tubal ligation over other methods. Economic barriers, a lack of education on the variety of methods available, and the fear of side effects contribute to a lower prevalence of hormonal contraception in India.
Several factors influence the choice of female contraception. Understanding the factors that drive the choice of contraception is essential for promoting reproductive health and ensuring that women have access to a range of effective and suitable contraceptive options. It also promotes public health goals, gender equity and improved well-being.