Breyanzi (lisocabtagene maraleucel) is a CD19-directed chimeric antigen receptor (CAR) T-cell immunotherapy indicated for the treatment of adult patients with relapsed or refractory (r/r) large B-cell lymphoma (LBCL), after first-line treatment.
Developed by US-based pharmaceutical company Bristol Myers Squibb (BMS), the personalised gene-modified autologous therapy holds the broadest patient eligibility for second-line LBCL, including diffuse large B-cell lymphoma (DLBCL), high-grade B-cell lymphoma (HGBCL), primary mediastinal large B-cell lymphoma (PMBCL), and follicular lymphoma grade 3B (FL3B).
In the US, a single dose of Breyanzi contains 90 to 110 x 10⁶ CAR-positive viable T cells for LBCL after one line of therapy, and 50 to 110 × 10⁶ CAR-positive viable T cells for LBCL after two or more lines of therapy. It is administered to the patients through a single intravenous transfusion.
In August 2025, the FDA granted priority review to BMS’s supplemental biologics licence application (sBLA) for Breyanzi for the treatment of adult patients with relapsed or refractory marginal zone lymphoma (MZL) who have undergone at least two previous systemic treatment regimens.
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of 5 December 2025.
Regulatory approvals for Breyanzi
The US Food and Drug Administration (FDA) provided the initial approval of Breyanzi for the treatment of adult patients with r/r LBCL following two or more lines of systemic therapy in February 2021, based on data from the TRANSCEND NHL 001 clinical trial.
In March 2021, Japan’s Ministry of Health, Labour and Welfare (MHLW) approved the drug for the treatment of patients with r/r LBCL and r/r follicular lymphoma (FL).
The European Commission (EC) approved Breyanzi for the treatment of adult patients with r/r DLBCL, PMBCL, and FL3B after two or more lines of systemic therapy in April 2022.
Breyanzi entered the second-line setting for the treatment of r/r LBCL in the US in June 2022 and in Japan in December 2022.
In May 2023, the EC approved Breyanzi for the treatment of adult patients with r/r DLBCL, HGBCL, PMBCL, and FL3B for second-line treatment.
In January 2024, the FDA approved two sBLAs for Breyanzi to expand into new indications, including treating adult patients with r/r FL and r/r mantle cell lymphoma (MCL) after a Bruton tyrosine kinase inhibitor (BTKi).
In March 2024, the FDA granted accelerated approval of Breyanzi for the treatment of adult patients with r/r chronic lymphocytic leukaemia (CLL) or small lymphocytic lymphoma (SLL) who have received at least two prior lines of therapy, including a Bruton tyrosine kinase inhibitor and a B-cell lymphoma 2 inhibitor.
In May 2024, the FDA approved Breyanzi for the treatment of adult patients with r/r FL who have received two or more prior lines of systemic therapy and for adult patients with r/r MCL who have received at least two prior lines of systemic therapy, including a BTK inhibitor.
The EC approved Breyanzi for the treatment of r/r FL who have received two or more prior lines of systemic therapy in March 2025, and for the treatment of adult patients with r/r MCL who have received at least two prior lines of systemic therapy, including a BTK inhibitor in November 2025.
Large B-cell lymphoma causes and symptoms
LBCL is a type of non-Hodgkin’s lymphoma (NHL) that originates in the lymphatic system and rapidly proliferates, primarily affecting B-cells, which are crucial for fighting infections.
Among its several subtypes, diffuse large B-cell lymphoma is the most prevalent form of NHL, followed by other common subtypes such as PMBCL and HGBCL.
Patients with LBCL may experience symptoms such as painless lymph node swelling, fever, night sweats, unintended weight loss, persistent fatigue, appetite loss, abdominal bloating due to an enlarged spleen, liver enlargement, itchy skin, and rashes.
The exact cause remains unknown, but risk factors include HIV, Epstein-Barr virus, a family history of NHL or HL, obesity, and chemical exposure. Diagnosis typically involves a biopsy of an enlarged lymph node or affected tissue.
CLL is a common adult leukaemia where abnormal lymphocytes accumulate in the bone marrow, impairing infection resistance and reducing healthy white and red blood cells and platelets. SLL also targets lymphocytes, with cancer cells predominantly found in lymph nodes.
FL, the second most common NHL and the leading subtype of indolent NHL, represents 20% to 30% of all NHL cases.
Typically diagnosed at the age of 65 years, FL involves white blood cells forming masses in lymph nodes or organs. Characterised by periods of remission and recurrence, FL becomes increasingly challenging to treat as it progresses.
MCL is a rare, aggressive form of NHL that accounts for 3% of all NHL cases. Originating from the mantle zone of the lymph node, MCL is more common in older adults and males.
Relapse after initial treatment is common, and the disease usually progresses or returns. MCL is considered incurable, with response rates and duration decreasing with each additional relapse.
Breyanzi’s mechanism of action
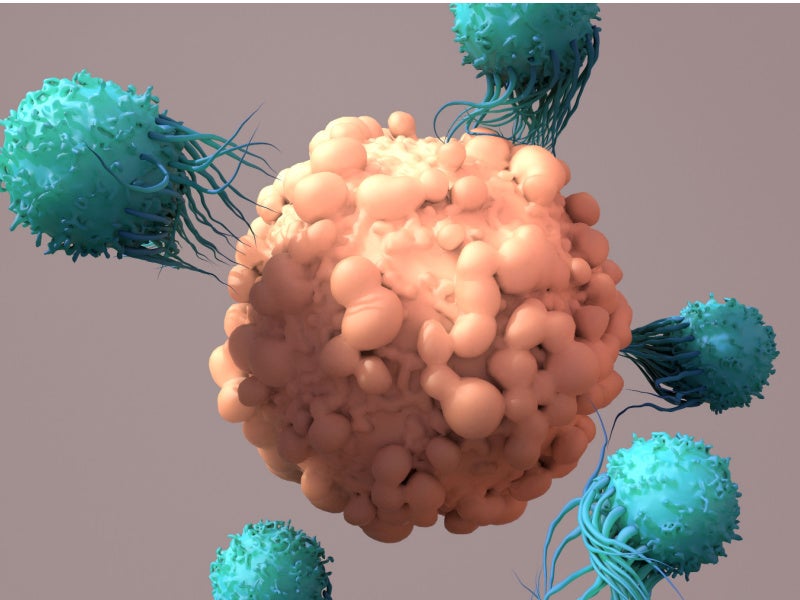
Breyanzi is a CAR T-cell therapy that specifically targets CD19 expressed on the cell surface of tumour and normal B cells.
The CAR contains an FMC63 monoclonal antibody-derived single-chain variable fragment, IgG4 hinge region, CD28 transmembrane domain, 4-1BB costimulatory domain, and CD3 zeta activation domain.
CD3 zeta signalling is important for initiating activation and anti-tumour activity while 4-1BB signalling promotes the expansion and persistence of the drug.
The CAR binds to CD19 and triggers the activation and proliferation of CAR T cells, leading to the release of proinflammatory cytokines and the cytotoxic death of cancer cells.
Clinical trials on Breyanzi
The TRANSCEND NHL 001 clinical trial was an open-label, multi-centre, multi-cohort, Phase I study assessing the safety, antitumour activity, and pharmacokinetics of Breyanzi in adults with r/r DLBCL, HGL, PMBCL, FL3B, and MCL.
The trial enrolled 268 participants with r/r LBCL who received Breyanzi, making it the largest pivotal trial for third-line plus r/r LBCL, encompassing a wide range of histologies and high-risk diseases.
Breyanzi was administered in both inpatient and outpatient settings. Of the 192 patients evaluated for efficacy, 73% responded to Breyanzi, with 54% achieving minimal or no detectable lymphoma post-treatment and 19% attaining a partial response.
The median response duration was 16.7 months for all responders. The median duration was not reached for patients who achieved a complete response (CR) while it stood at 1.4 months for patients with a partial response.
Among 104 patients who reached a CR, 65% had remissions lasting at least six months, and 62% had remissions of at least nine months.
The Phase III TRANSFORM clinical trial, another significant study, was a global, randomised, open-label, multicentre trial comparing Breyanzi to standard-of-care (SOC) regimens, including high-dose chemotherapy and haematopoietic stem cell transplant in adults with r/r LBCL post-first-line chemotherapy.
The trial randomised 184 patients equally to receive either a single infusion of Breyanzi or the SOC. The primary endpoint was event-free survival (EFS), with progression-free survival (PFS) also assessed.
Patients treated with Breyanzi had a median EFS of 10.1 months, significantly longer than the 2.3 months observed in the SOC arm.
Breyanzi achieved a CR in 66% of patients, compared to 39% in the SOC arm, and more than double the PFS. The safety profile of Breyanzi was well-established in the study.
Additional clinical trials of Breyanzi
The Phase II PILOT single-arm, open-label, multi-centre trial assessed Breyanzi as a second-line treatment for transplant-ineligible patients with r/r LBCL.
The study included a diverse patient population based on age, performance status, organ function, and comorbidities, without restrictions on relapse timing after first-line therapy.
Breyanzi achieved an overall response rate (ORR) of 80%, the primary endpoint, and a CR rate of 54%.
The median time to CR was one month (range: 0.8 to 6.9 months), and the median duration of response stood at 11.2 months. Patients who attained a CR did not reach the median duration of response.
Adverse events commonly reported were cytokine release syndrome (CRS), fever, fatigue, musculoskeletal pain, and nausea.
In the TRANSCEND CLL 004 Phase I/II, open-label, single-arm trial, Breyanzi was investigated for adults with r/r CLL or SLL.
The primary endpoints included the response rate and duration of response. Approximately 20% of patients achieved a CR, with the median duration of CR pending, while the safety profile remained consistent.
The TRANSCEND FL Phase II single-arm global, multi-centre study evaluated Breyanzi in patients with r/r indolent B-cell NHL, including FL.
The primary outcome measure focused on the ORR, which encompassed the best overall response of complete or partial response post-lisocabtagene maraleucel infusion, and the duration of response (DOR).
The ORR reached 95.7%, and after a median follow-up of 16.8 months, the median DOR was not achieved.
The most frequent adverse reactions included CRS, headache, musculoskeletal pain, fatigue, constipation, and fever.