Crysvita® (burosumab-twza) is a fibroblast growth factor 23 (FGF23) blocking antibody indicated for the treatment of X-linked hypophosphatemia (XLH) in adults and children.
Available for patients in the US, Europe and Canada, the drug is jointly developed and marketed by Kyowa Hakko Kirin and Ultragenyx Pharmaceutical. The firms submitted a biologics license application (BLA) to the Food and Drug Administration (FDA) in August 2017.
Crysvita was approved by the European Commission (EC) for the treatment of XLH with radiographic evidence of bone disease in children aged one year and older in February 2018. The FDA approved the drug for the treatment of XLH in adults and children aged one year and older in April 2018, while Health Canada approved the drug in December 2018.
The companies submitted an application for the manufacturing and marketing of Crysvita to treat FGF23-related hypophosphatemic rickets and osteomalacia in Japan in January 2019. An approval from Japan’s Ministry of Health, Labour and Welfare is expected in September 2019.
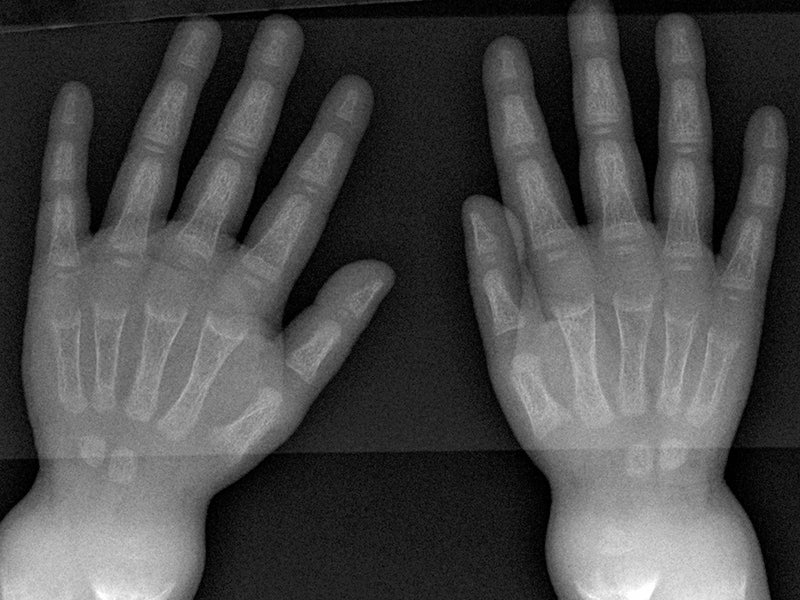
XLH causes and symptoms
XLH is a rare hereditary skeletal disorder that causes renal phosphate wasting in children and adults due to excessive production of the FGF23 protein. This reduces the reabsorption of renal tubular phosphate and production of 1,25 dihydroxy vitamin D.
The disease leads to hypophosphatemia, which is a deficiency of phosphorus in the patient’s blood that gradually softens and weakens the bones. XLH affects approximately 3,000 children and 12,000 adults in the US.
Common symptoms of the disease in children are rickets, short stature, bone pain, severe dental pain and bone deformities. In adults, the disease causes osteomalacia, which increases the risk of bone fractures in patients.
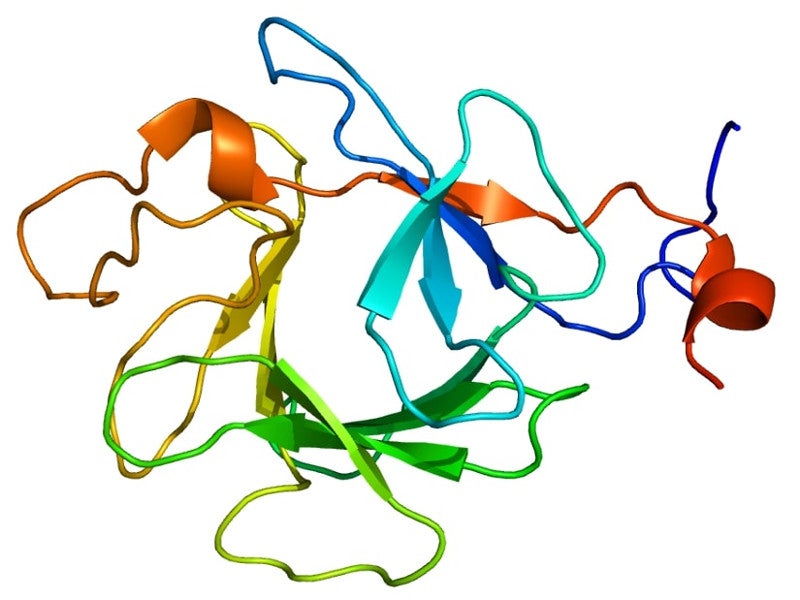
Crysvita’s mechanism of action
Crysvita is a recombinant human monoclonal IgG1 antibody that binds to and blocks the biological activity of FGF23 protein. It restores renal tubular phosphate reabsorption and increases the production of 1,25 dihydroxy vitamin D, which enhances the absorption of phosphate and calcium in the intestine of patients with XLH.
The drug is available as a sterile solution that can be clear to slightly opalescent in colour. Designed for subcutaneous administration, it is available in 10mg/ml, 20mg/ml and 30mg/ml dosage strengths in a single-dose vial.
Clinical studies on Crysvita
The FDA’s approval of Crysvita was based on the results of two Phase II clinical studies conducted on paediatric patients and two Phase III studies conducted on adult patients.
A total of 65 paediatric patients with XLH were enrolled in two Phase II clinical trials to study the safety and efficacy of the drug. Out of 65 patients, 52 were enrolled for Study 1 and the remaining for Study 2.
Study 1 was a 48-week, randomised, open-label study, while Study 2 was a 64-week open-label study. Normal phosphorus level was demonstrated in 94%-100% of children administered with Crysvita in the two clinical trials.
Two Phase III clinical trials were performed in adults with XLH, named Study 3 and Study 4. Study 3 was a 24-week placebo-controlled, randomised, double-blind clinical study that enrolled 134 adult patients. Study 4 was a 48-week open-label, single-arm study that enrolled 14 adult XLH patients to assess the effect of the drug in improving osteomalacia.
In Study 3, 94% of patients treated with Crysvita achieved normal phosphorus level compared to just 8% of those who received placebo, while improved osteomalacia was observed in ten patients in Study 4.
A Phase III 64-week, randomised, active-controlled clinical study that enrolled 61 children with XLH was also conducted. The efficacy and safety of Crysvita in patients were compared with those in conventional therapy, including oral phosphate and active vitamin D.
The primary endpoint was a change in rickets at week 40. The patients treated with Crysvita demonstrated significant improvement in rickets severity and physical functioning.