Ebanga™ (ansuvimab-zykl) is a Zaire ebolavirus glycoprotein (EBOV GP) directed human monoclonal antibody for the treatment of Zaire ebolavirus infection in adult and paediatric patients. Neonates born to mothers who test reverse transcription polymerase chain reaction (RT-PCR) positive for the infection are also eligible for the treatment.
The drug was originally developed by the Vaccine Research Centre of the National Institute of Allergy and Infectious Diseases (NIAID), part of the US Government’s National Institutes of Health (NIH).
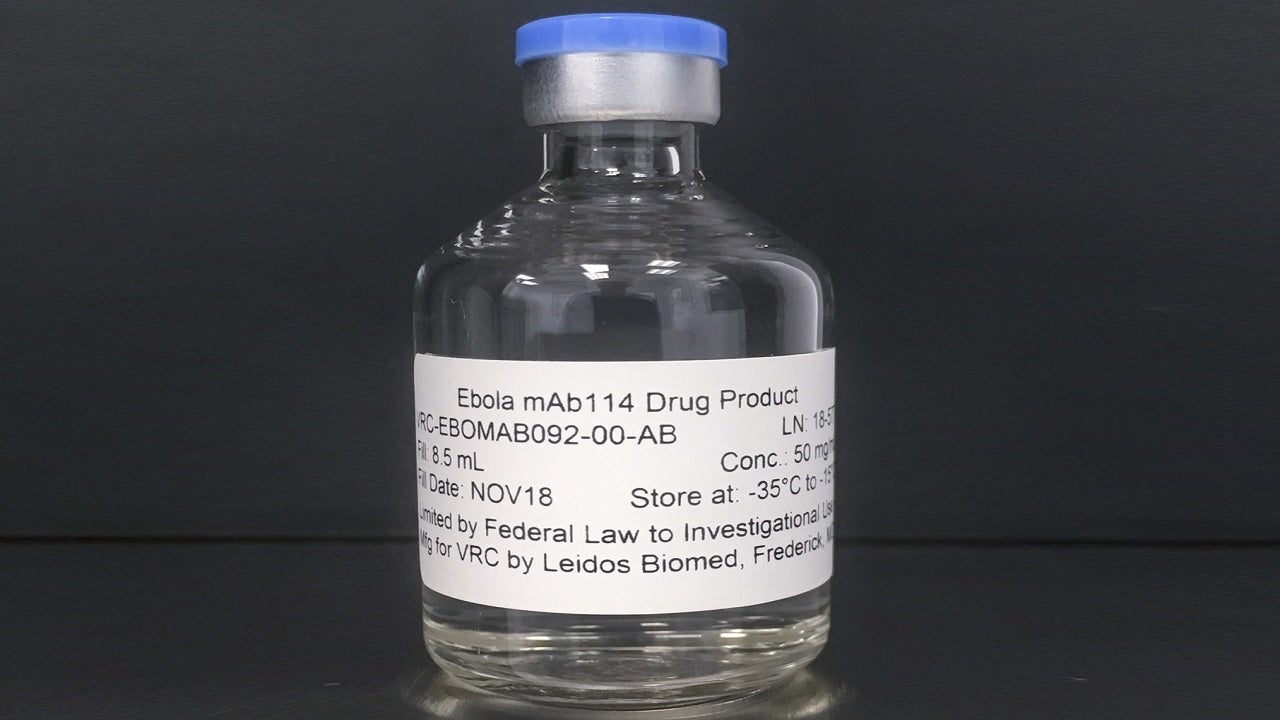
In December 2018, US-based biotechnology company Ridgeback Biotherapeutics received a licence for Ebanga (formerly known as mAb114) from the NIAID under a patent license agreement for intellectual property associated with the monoclonal antibody.
Ebanga is available as 400mg of ansuvimab-zykl in a single-dose vial as an off-white to white lyophilised powder for reconstitution for intravenous administration.
Ebanga approvals
Ebanga was granted orphan drug designation and breakthrough therapy designation by the US Food and Drug Administration (FDA) for Ebola treatment in May 2019 and September 2019 respectively.
In April 2020, Ridgeback secured a $10.9m contract from the US Biomedical Advanced Research and Development Authority (BARDA) for the development of ansuvimab for the treatment of Ebola virus disease.
The therapy’s development has been wholly or partially funded by the proceeds from the US Department of Health and Human Services (HHS), as well as the Office of the Assistant Secretary for Preparedness and Response (ASPR) and BARDA.
In May 2020, Ridgeback submitted a biologics license application (BLA) for Ebanga to the FDA. This was accepted under priority review in July 2020.
In August 2020, Ridgeback began an expanded access protocol for the rapid accessibility of Ebola treatment, ansuvimab, in the Democratic Republic of the Congo (DRC).
In December 2020, the FDA approved the drug for the treatment of Zaire ebolavirus infection in adults and children, including newborns whose mothers had tested positive for the infection.
Ebanga is the second FDA-approved drug for the treatment of Zaire ebolavirus infection after Regeneron’s Inmazeb™ (atoltivimab, maftivimab and odesivimab-ebgn), a triple monoclonal antibody cocktail drug approved in October 2020.
Zaire ebolavirus infection causes and symptoms
Ebola, or Ebola virus disease (EVD), also called Zaire ebolavirus infection, is an infection caused by Zaire ebolavirus, one of four Ebolavirus species. EVD is a rare but severe, often fatal disease in humans, and is endemic to the African continent.
The infection is caused by a group of viruses within the Ebolavirus genus. The virus is transmitted through direct contact with the blood or objects contaminated with the body fluids of an infected person who has symptoms or has died from Ebola.
EVD is transmitted from wild animals to humans and spreads throughout the human population via human-to-human transmission. If left untreated, the Ebola virus can cause an acute and severe infection, which is often lethal.
The symptoms usually appear between two and 21 days after contact with the virus. The symptoms of the disease include weakness, headache, muscle pain, stomach pain, fever, diarrhoea, vomiting, sore throat, unexplained bleeding, haemorrhaging and bruising.
Ebanga’s mechanism of action
Ebanga (ansuvimab-zykl) is a recombinant human monoclonal antibody that exhibits antiviral activity against Zaire ebolavirus. It is produced using recombinant DNA technology in Chinese hamster ovary (CHO) cells.
The drug binds to glycoprotein expressed on the surface of the Ebola virus and inhibits the virus’ attachment and entry into the host cells. It blocks the binding between the Ebola virus glycoprotein, EBOV GP1, and the Niemann-Pick C1 (NPC1) receptor on host cells by binding to the LEIKKPDGS epitope located on the receptor-binding site of the GP1 subunit, thereby inhibiting the virus’ entry into the host cell.
Clinical trials on Ebanga
The FDA’s approval of Ebanga was based on the outcome of a multi-centre, open-label, randomised, controlled clinical trial, Pamoja Tulinde Maisha (PALM).
The PALM trial was led by the US National Institutes of Health and the Institut National de Recherche Biomédicale and involved many other international organisations and agencies. It was carried out during an Ebola outbreak in the DRC between 2018 and 2019.
The trial evaluated Ebanga’s safety and efficacy in patients with confirmed Zaire ebolavirus infection, including adults and children. The patients were randomised to receive either Ebanga intravenously as a single infusion, or an investigational control.
In the study, 174 participants received a single intravenous dose of 50mg/kg Ebanga, while 168 participants received an investigational control.
The PALM trial’s primary efficacy endpoint was the mortality rate at day 28. Results showed that 35.1% of the patients who received Ebanga died after 28 days, compared to 49.4% of the patients in the control arm.
Common adverse events reported in patients during the clinical trial were fast heart rate, fever, fast breathing, chills, hypotension, vomiting and diarrhoea. The FDA noted that the treatment should not be administered in combination with a live virus vaccine against the Ebola virus.