Gavreto™ (pralsetinib) is a targeted therapy indicated for the treatment of metastatic rearranged during transfection (RET) fusion-positive non-small cell lung cancer (NSCLC), diagnosed by a US Food and Drug Administration (FDA)-approved test, in adult patients.
Blueprint Medicines developed the therapy, which entered a global collaboration with Roche and its subsidiary Genentech for the development and commercialisation of Gavreto for RET-altered cancers, different forms of thyroid cancer and other solid tumours in July 2020.
Blueprint Medicines and Genentech will jointly commercialise Gavreto in the US. Roche will obtain an exclusive license to market the drug outside the US, excluding Greater China.
Blueprint partnered with CStone Pharmaceuticals for the development and commercialisation of Gavreto in Greater China that includes Mainland China, Hong Kong, Macau and Taiwan.
Blueprint selected PANTHERx® Rare Pharmacy as a limited distribution partner for the drug.
Gavreto is Blueprint Medicines’ second breakthrough therapy, which obtained FDA approval after AYVAKIT™ (avapritinib) in 2020.
The therapy will be available as light blue, opaque, hard hydroxypropyl methylcellulose (HPMC) capsules in 100mg dose strength for oral administration.
Gavreto approvals
The US Food and Drug Administration (FDA) accepted the marketing application for pralsetinib for the treatment of RET fusion-positive NSCLC in May 2020.
Blueprint Medicines submitted a new drug application (NDA) for pralsetinib to the FDA for the treatment of advanced RET mutant medullary thyroid cancer (MTC) and RET fusion-positive thyroid cancers in July 2020.
Gavreto received accelerated approval for the treatment of RET fusion-positive NSCLC in adult patients in September 2020. The NDA for the treatment of MTC and thyroid cancers received priority review under the FDA’s Real-Time Oncology Review (RTOR) pilot programme in the same month, with a target action date set as February 2021.
The European Medicines Agency validated Gavreto for marketing in Europe for the treatment of RET fusion-positive NSCLC.
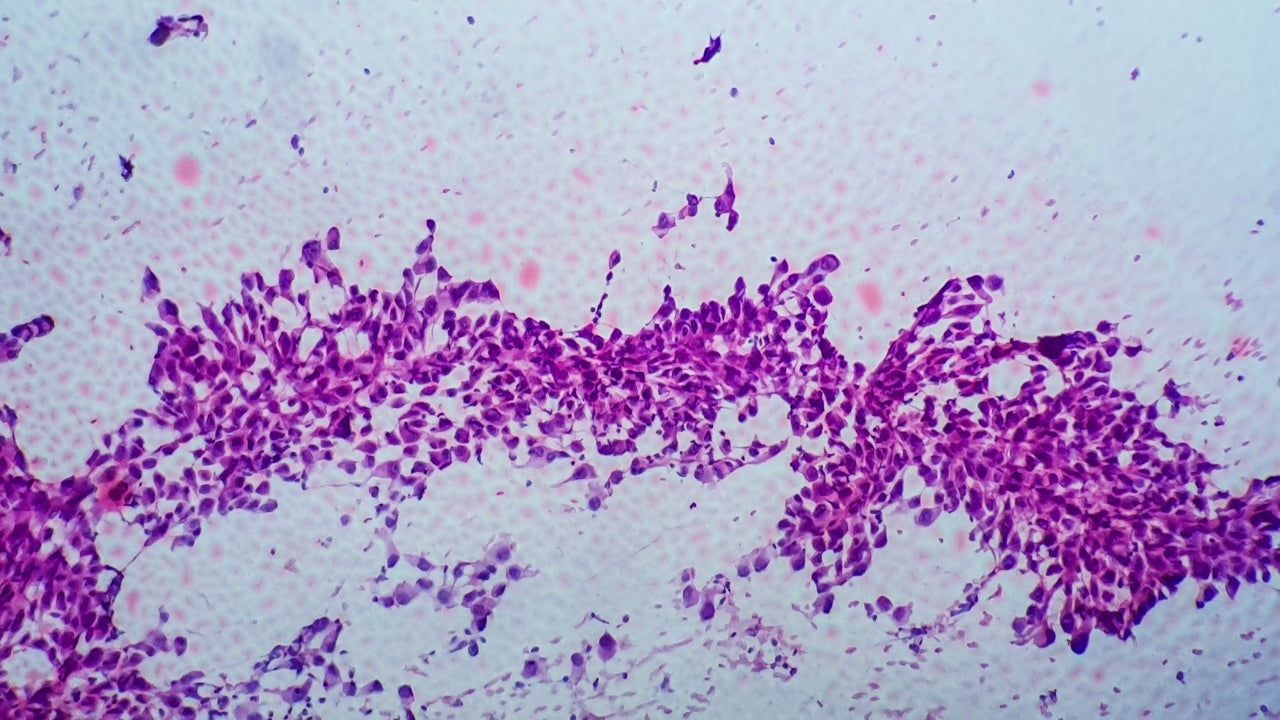
Non-small cell lung cancer (NSCLC) causes and symptoms
Non-small cell lung cancer (NSCLC) is a type of lung cancer that accounts for approximately 80%-85% of all lung cancers.
RET fusion affects between 1% and 2% of NSCLC patients and between 10% and 20% of patients with papillary thyroid cancer, while RET mutations appear in approximately 90% of patients with advanced MTC.
Low-frequency oncogenic RET fusions are found in colorectal, breast, pancreatic and other cancers, as well as in NSCLC EGFR-mutant patients resistant to therapy.
NSCLC’s symptoms include chest pain, persistent coughing, wheezing, bloody sputum, shortness of breath, swollen neck or face, fatigue, unintentional weight loss, impaired voice and appetite loss.
Pralsetinib mechanism of action
Pralsetinib is a once-daily, oral precision therapy, which selectively targets cancer-causing RET alterations. It is a wild-type RET and oncogenic RET fusion (CCDC6-RET) and mutation (RET V804L, RET V804M, and RET M918T) kinase inhibitor at lower concentrations.
It inhibits with a half maximum inhibitory concentration (IC50s) of less than 0.5nM.
The drug specifically suppresses RET changes that cause multiple forms of cancer.
Prelsetinib demonstrated anti-cancer activity in cultured cells and animal tumour implantation models including oncogenic RET fusions or mutations, such as KIF5B-RET, CCDC6-RET, RET M918 T, RET C634W, RET V804E, RET V804L and RETV804M.
Clinical trials on Gavreto
FDA approval of Gavreto comes from the outcomes of a phase one / two open-label, non-randomised, multi-centre, multi-cohort clinical trial named ARROW.
Next-generation sequencing (NGS), in situ fluorescence hybridisation (FISH) and other tests detected the RET-gene fushions.
A total of 114 patients enrolled in two separate cohorts. One cohort had 87 patients with metastatic RET fusion-positive NSCLC whose cancer progressed on platinum-based chemotherapy, while the other cohort had 27 previously untreated metastatic NSCLC patients.
Primary goals of the study were overall response rate (ORR) and duration of response (DOR).
The recruited patients received 400mg of Gavreto once daily until disease progression or unacceptable toxicity.
The cohort with previously treated NSCLC showed an ORR of 57%, while the median duration of response in them was not estimable. 5.7% of the patients demonstrated complete response, while 52% of the patients showed a partial response to the therapy. A total of 80% of the patients demonstrated a DOR of six months or more.
ORR was 70% in the other cohort with previously untreated metastatic NSCLC patients. 11% of the patients showed a complete response, while 59% of the patients showed a partial response to the therapy.
The median DOR was nine months with 58% of patients showing a DOR of at least six months.
Common side effects of Gavreto observed in patients included constipation, muscle pain fatigue, high blood pressure, decreased neutrophils and lymphocytes, decreased haemoglobin, decreased phosphate, decreased calcium, decreased sodium, and increased alanine aminotransferase (ALT).