IMCIVREE® (setmelanotide) is indicated for chronic weight management in adult and paediatric patients aged six years and older with monogenic or syndromic obesity due to three rare genetic conditions, namely proopiomelanocortin (POMC) deficiency, proprotein convertase subtilisin/kexin type 1 (PCSK1) deficiency or leptin receptor (LEPR) deficiency or Bardet-Biedl syndrome (BBS).
Developed by Rhythm Pharmaceutical, IMCIVREE is available as 10mg/ml clear to slightly opalescent, colourless to faintly yellow solution in a 1ml multiple-dose vial for subcutaneous injection.
In July 2021, Rhythm Pharmaceutical collaborated with Medison Pharma to commercialise IMCIVREE in Israel.
The company also entered an exclusive licencing agreement with RareStone, a biopharmaceutical company based in China, for developing and marketing the drug in China in December 2021.
Regulatory approvals for IMCIVREE
In March 2020, Rhythm submitted a new drug application (NDA) for the drug to the US Food and Drug Administration (FDA) for the condition. A supplemental NDA was later submitted to the FDA for the treatment of obesity and control of hunger in adult and paediatric patients with Bardet-Biedl syndrome (BBS) or Alström syndrome in September 2021.
IMCIVREE was initially approved in November 2020, becoming the first-ever FDA-approved treatment for the rare genetic diseases of obesity. In June 2022, it was granted approval for chronic weight management in patients with monogenic and syndromic obesity due to BBS.
The FDA has also granted setmelanotide the rare paediatric disease designation for treating POMC and LEPR-deficient obesities.
The company filed a marketing authorisation application (MAA) to the European Medicines Agency (EMA) in July 2020.
In May 2021, the Committee for Medicinal Products for Human Use (CHMP) issued a favourable opinion for IMCIVREE’s approval in Europe. The European Commission (EC) approved the drug for treating obesity and hunger control associated with POMC, PCSK1, and LEPR deficiency in July 2021.
The drug is also designated as an orphan medicinal product and was granted eligibility for the priority medicines (PRIME) scheme in Europe.
In September 2021, the UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) granted marketing authorisation to IMCIVREE. The following month, Rhythm submitted a Type II variation application to the EMA for approving the drug for Bardet-Biedl and Alström syndromes.
Causes and symptoms of obesity
Obesity is a complex condition that may be driven by a combination of genetic, behavioural, metabolic or lifestyle factors.
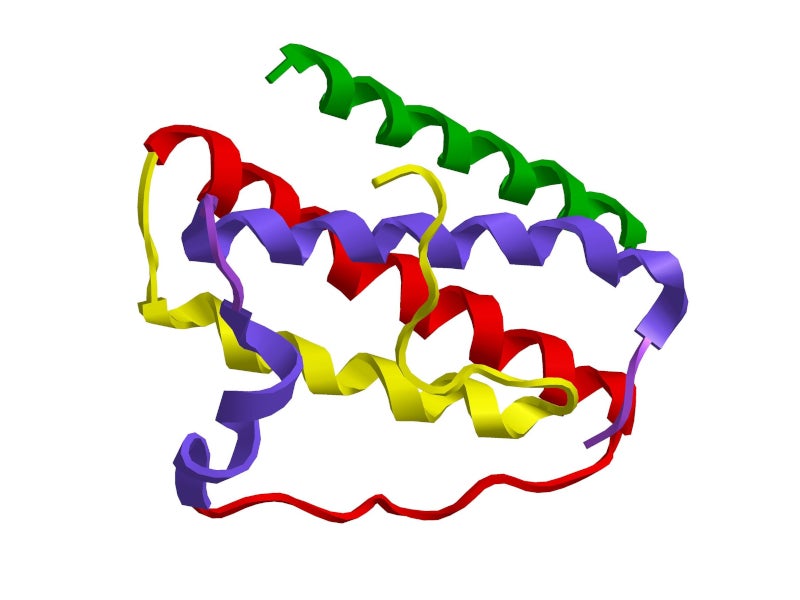
Obesity caused due to POMC, PCSK1 or LEPR deficiency is an ultra-rare disease. In these conditions, variants of the POMC, PCSK1 or LEPR genes impair the MC4 receptor pathway, which is responsible for the regulation of hunger, metabolism and body weight.
Monogenic obesity is caused by a single gene mutation, mainly in the leptin-melanocortin pathway, resulting in POMC, PCSK1 or LEPR deficiency.
Syndromic obesity is linked to a variety of phenotypes, the most common of which are BBS and Prader Willi syndrome, both of which cause severe obesity by impairing the MC4 receptor pathway. From early in life, children with the condition exhibit an increased appetite, endocrine issues, red hair, and pale skin colour.
Obese people are prone to developing heart disease and strokes, Type 2 diabetes, certain cancers, digestive issues, sleep apnoea, and osteoarthritis.
IMCIVREE’s mechanism of action
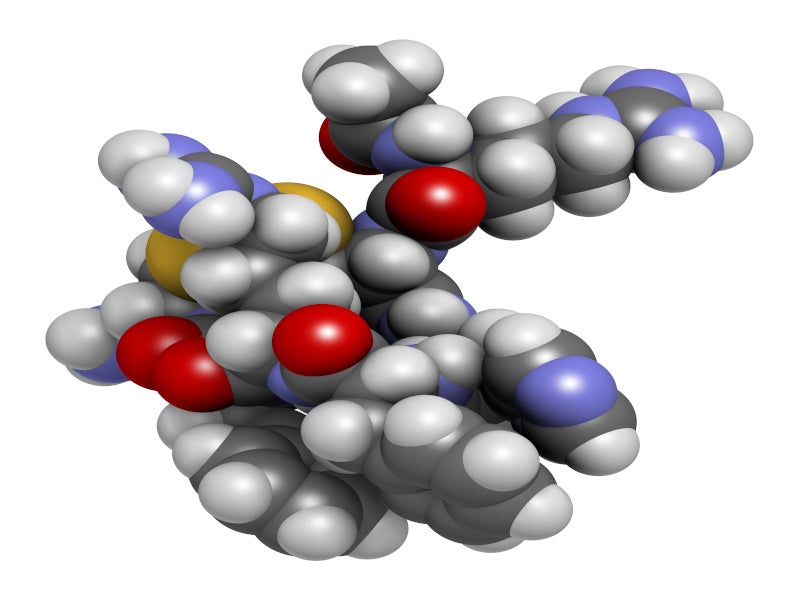
Setmelanotide is an MC4 receptor agonist with 20 times less activity at the melanocortin 3 (MC3) and melanocortin 1 (MC1) receptors.
IMCIVREE helps stimulate MC4 receptor pathway activity to reduce hunger and promote weight loss by decreasing caloric intake and increasing energy expenditure in patients with obesity due to POMC, PCSK1, or LEPR deficiencies.
Clinical trials on IMCIVREE
IMCIVREE’s efficacy and safety were studied in two Phase III, identically designed, one-year, open-label clinical trials, each of which had an eight-week, double-blind withdrawal period.
Study I enrolled patients aged six years and older with obesity and genetically confirmed or suspected POMC or PCSK1 deficiency, while Study II enrolled patients aged six years and older with obesity and genetically confirmed or suspected LEPR deficiency.
Both trials’ primary endpoint was a 10% drop in body weight from baseline after 52 weeks of therapy.
IMCIVREE’s efficacy was evaluated in 21 recruited patients, ten of whom were enrolled in Study I and 11 in Study II, who had completed at least one year of treatment. An additional six patients, four being in Study I and two in Study II, were also enrolled before they had completed one year of treatment.
In Study I, 80% of patients with obesity due to POMC or PCSK1 deficiency achieved at least 10% weight loss in one year, while in Study II, 46% of patients with obesity due to LEPR deficiency met the primary endpoint.
The most common adverse conditions reported in patients during the trials were injection site reactions, skin hyperpigmentation, nausea, headache, diarrhoea, pain in the abdomen, back pain, fatigue, vomiting, depression, upper respiratory tract infection, and spontaneous penile erection.