Juluca® (Dolutegravir and Rilpivirine) is a two-drug regimen indicated for the maintenance treatment of HIV-1 infection in adults.
The drug was developed by ViiV Healthcare in association with Pfizer and Shionogi. GlaxoSmithKline holds a majority stake in ViiV Healthcare.
Submitted to the US Food and Drug Administration (FDA) in June 2017, a new drug application (NDA) for Juluca® was approved in November 2017. The company also submitted marketing applications (MA) in Europe, Canada, Australia and Switzerland.
Juluca® received positive opinion for the approval from the European Medicines Agency’s (EMA) Committee for Human use of Medicinal Products (CHMP) in March 2018.
The European Commission (EC) granted marketing authorisation (MA) approval for the drug in May 2018. It was also approved in Canada in May 2018.
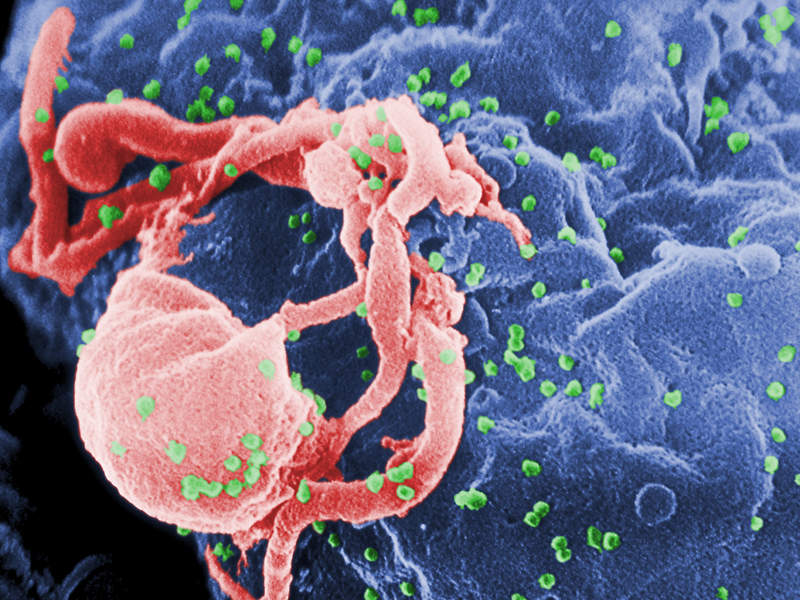
HIV-1 Infection causes and symptoms
Human immunodeficiency virus (HIV) is a lentivirus that causes HIV infection, which is responsible for causing acquired immune deficiency syndrome (AIDS).
HIV-1 and HIV-2 are two types of HIV virus. HIB-1 is more virulent and infective than HIV-2.
Symptoms associated with HIV-1 infection include fever, fatigue, pharyngitis, weight loss, night sweats, lymphadenopathy, myalgias, headache, nausea and diarrhoea.
An estimated 36.7 million people worldwide are living with HIV, while approximately 1.8 million people are newly infected each year.
Juluca’s mechanism of action
Juluca® comprises 50mg of integrase strand transfer inhibitor dolutegravir and 25mg of non-nucleoside reverse transcriptase inhibitor rilpivirine.
The drug restrains HIV integrase by binding to the integrase active site and stopping the strand transfer step of retroviral DNA integration. It also restrains HIV-1 replication by non-competitive inhibition of HIV-1 reverse transcriptase (RT).
The drug is available in tablet form for oral administration.
Clinical trials on Juluca
The FDA’s approval for Juluca® was based on results obtained from two pivotal Phase III clinical trials named SWORD. The studies enrolled more than 1,000 patients that previously achieved stable viral suppression for at least six months on other anti-retroviral regimens.
The clinical trials were open-label, randomised, multi-centre, non-inferiority studies designed to assess the safety and efficacy of switching to the two-drug regimen of dolutegravir and rilpivirine compared with remaining on an antiretroviral regimen (CAR).
The studies were conducted for 48 weeks and are expected to be continued for a further 148 weeks.
The primary endpoint of the studies was the achievement of plasma HIV-1 rebinucleaic acid (RNA) copies at less than 50 per millilitre at week 48. The secondary endpoints included the development of viral resistance, safety and tolerability, as well as changes in renal, bone and cardiovascular biomarkers.
The results indicated that patients treated with Juluca® achieved non-inferior viral suppression at 48 weeks compared with a three-drug CAR in both studies. The proportion of patients who discontinued treatment due to adverse events (AE) was 4% in the Juluca® administered group, compared with less than 1% in the three-drug CAR group.
The results also showed that patients treated with Juluca® saw a neutral effect on lipids at week 48. It was reported that total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, and total cholesterol to HDL ratio was same across the treatment arms.
In addition, the studies found that the mean bone mineral density (BMD) increased from baseline to week 48 in people who changed from an antiretroviral treatment (ART) regimen containing tenofovir disoproxil fumarate (TDF) to Juluca®.
The most common AEs reported that led to the discontinuation of treatment in the Juluca® administered group were psychiatric disorders, diarrhoea and headaches.