Loqtorzi (toripalimab-tpzi) is an immuno-oncology therapy indicated in combination with cisplatin and gemcitabine combination chemotherapy for the first-line treatment of adult patients with metastatic or recurrent locally advanced nasopharyngeal carcinoma (NPC).
It is also eligible as a monotherapy for patients with recurrent, unresectable, or metastatic NPC with disease progression on or after platinum-containing chemotherapy.
Developed jointly by Coherus Biosciences, a US-based biopharmaceutical company and Junshi Biosciences, a biopharmaceutical company based in China, Loqtorzi is a next-generation, anti-programmed death receptor-1 (PD-1) monoclonal antibody.
Toripalimab was initially developed by Junshi. Coherus acquired the rights to develop and market toripalimab in the US and Canada through a licensing agreement struck in February 2021.
In January 2024, Inovio, a biotechnology company based in the US, collaborated with Coherus to evaluate its drug candidate INO-3112 in combination with Loqtorzi as a potential treatment for locoregionally advanced, high-risk, HPV16/18 positive oropharyngeal squamous cell carcinoma, a type of head and neck cancer commonly known as throat cancer.
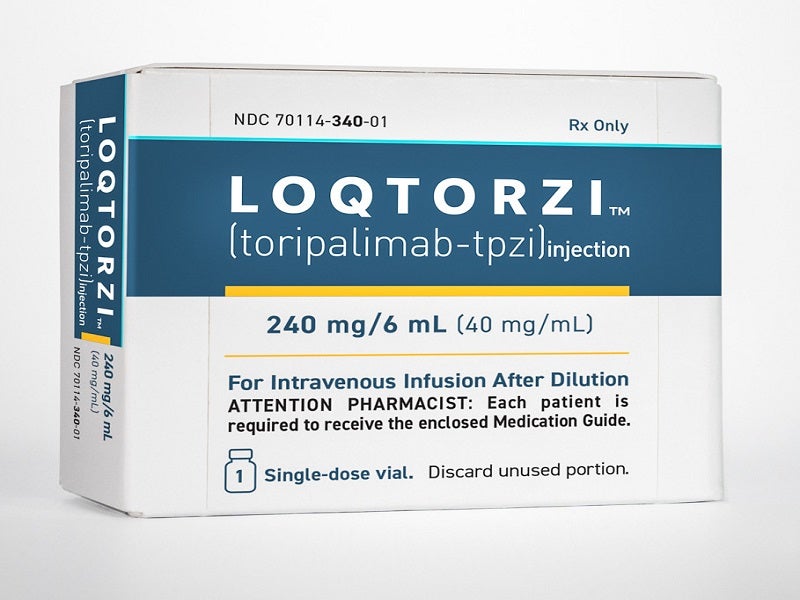
Loqtorzi is available in 240mg/6ml dosage strength as a sterile, preservative-free, clear to slightly opalescent, colourless to slightly yellow solution supplied in a single-dose vial for intravenous use.
Regulatory approvals for Loqtorzi
Loqtorzi received the US Food and Drug Administration’s (FDA) approval in combination with chemotherapy for the treatment of metastatic or recurrent locally advanced NPC and as a monotherapy in October 2023.
The drug was made available in the US in January 2024 through select speciality distributors.
NPC causes and symptoms
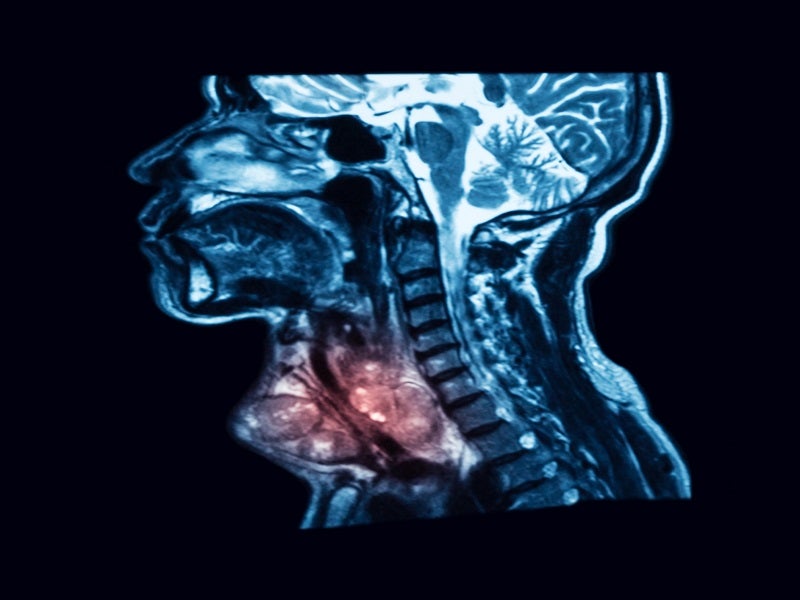
NPC is a rare type of head and neck cancer occurring in the nasopharynx, located in the upper part of the throat behind the nose.
It is difficult to detect the disease in the early stages as the nasopharynx is hard to examine.
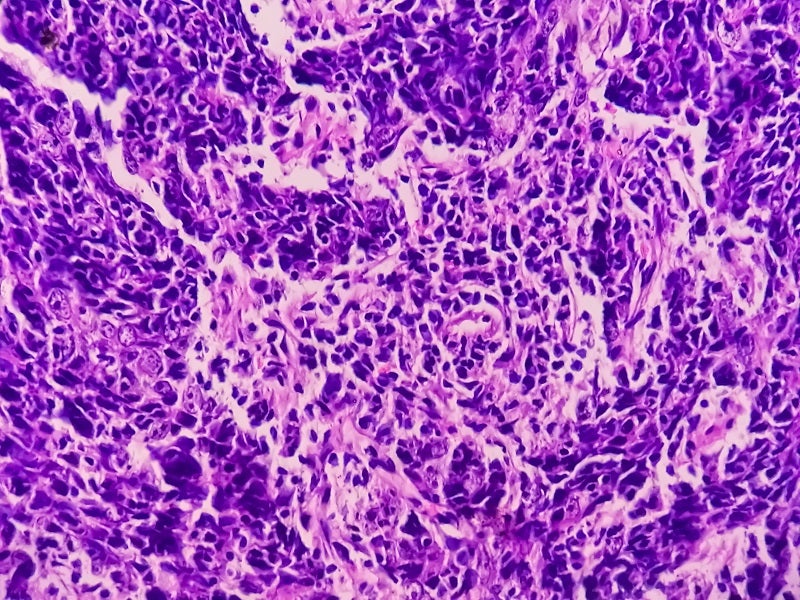
The disease develops when cells in the nasopharynx grow abnormally and form cancerous tumours that can spread to lymph nodes, liver, lungs, and bones.
Surgery is a rare option due to the tumour’s location in the back of the nose and mouth.
Treatment for patients with localised NPC usually includes radiation therapy, chemotherapy, or a combination of both.
The exact cause of the disease is unknown. Lifestyle behaviours and medical conditions are, however, the probable reasons for developing the condition.
Some of the causes include heavy smoking, frequent consumption of alcohol, salt-cured foods, the Epstein-Barr virus, consistent exposure to dust and smoke, family history, race, and sex.
The most common symptoms include a painless lump on the back of the neck, tinnitus, hearing loss, ear infections, headaches, stuffy nose, nose bleeds, difficulty breathing and opening of the mouth, facial pain, and numbness.
NPC is rare in the US and occurs much more commonly in other parts of the world, specifically in Southeast Asia. The five-year survival rate for patients with NPC is approximately 60%. Patients with the progressed disease have a five-year survival rate of about 49%.
Loqtorzi’s mechanism of action
Loqtorzi is an anti-PD1 humanised IgG4 monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2 ligands at a specific location with high affinity releasing PD-1 pathway-mediated inhibition of the immune response.
It enables the immune system to attack and kill tumour cells. It also demonstrates improvement in the overall survival of cancer patients with various tumour types.
Clinical trials on Loqtorzi
The FDA approval of Loqtorzi was based on data from pivotal Phase III JUPITER-02 and Phase II POLARIS-02 clinical trials and is irrespective of a patient’s PD-L1 status.
JUPITER-02 is a multicentred, randomised, double-blinded, placebo-controlled, multinational study to evaluate a checkpoint inhibitor plus chemotherapy for the first-line treatment of recurrent or metastatic NPC.
The study enrolled 289 patients with metastatic or recurrent, locally advanced NPC who had not received previous systemic chemotherapy for recurrent or metastatic disease.
Patients were randomised in a 1:1 ratio to receive either 240mg Loqtorzi or placebo in combination with gemcitabine and cisplatin every three-week treatment cycle, followed by toripalimab-tzpi or placebo monotherapy every three weeks until disease progression, intolerable toxicity, or two years of treatment completion.
Progression-free survival (PFS) was the primary endpoint of the study. In the study, Loqtorzi successfully achieved the primary endpoint by showcasing a significant improvement in PFS when compared to the chemotherapy-alone group using toripalimab-tzpi.
It resulted in a substantial 48% reduction in the risk of disease progression or mortality. The positive impact on PFS was consistent regardless of the PD-L1 status.
Loqtorzi demonstrated a statistically significant and clinically meaningful improvement in overall survival (OS) with treatment, resulting in a 37% reduction in the risk of death versus chemotherapy alone. Loqtorzi demonstrated a good safety and tolerability profile with the PD-1 inhibitor class.
The drug also demonstrated progress in overall response rate (ORR), duration of response, and disease control rate (DCR), where 77% of patients treated with Loqtorzi exhibited a complete or partial response of 19% and 58%, respectively.
The patients receiving Loqtorzi achieved a median response duration of ten months, whereas it was 5.7 months in the chemotherapy-alone group.
The most common adverse events reported during the study were nausea, vomiting, decreased appetite, constipation, hypothyroidism, rash, pyrexia, diarrhoea, peripheral neuropathy, cough, musculoskeletal pain, upper respiratory infection, insomnia, dizziness, and malaise.
The POLARIS-02 clinical study assessed the efficacy of toripalimab-tpzi as a monotherapy. It is an open-label, multicentre, single-country, multi-cohort trial, which enrolled 172 patients with unresectable or metastatic NPC who had received prior platinum-based chemotherapy or had disease progression within six months of completing platinum-based chemotherapy.
In the study, Loqtorzi demonstrated a lasting anti-tumour action in patients with recurrent or metastatic NPC who failed earlier chemotherapy. The study showed an objective response rate of 20.5%, a DCR of 40.0%, and a median OS of 17.4 months with a considerable safety profile.
The most common adverse reactions were hypothyroidism, fatigue, and cough.