OJEMDA™ (tovorafenib) is a novel treatment indicated for patients aged six months and older with relapsed or refractory paediatric low-grade glioma (pLGG) with a BRAF fusion or rearrangement, or a BRAF V600 mutation – the most prevalent molecular alteration in pLGG.
The drug is developed by Day One Biopharmaceuticals, a biopharmaceutical company based in the US. The company partnered with the National Cancer Institute’s (NCI) Division of Cancer Treatment and Diagnosis, Cancer Therapy Evaluation Program through a cooperative research and development agreement to broaden research opportunities for tovorafenib in October 2022.
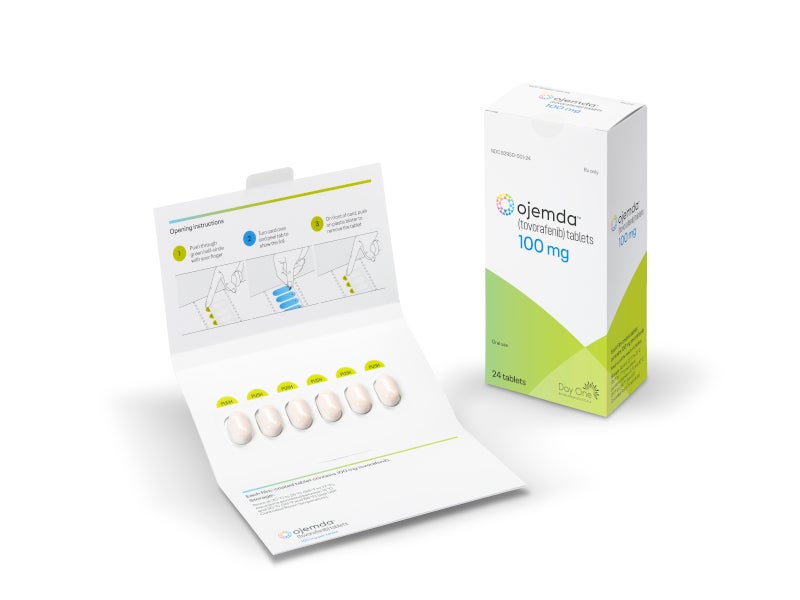
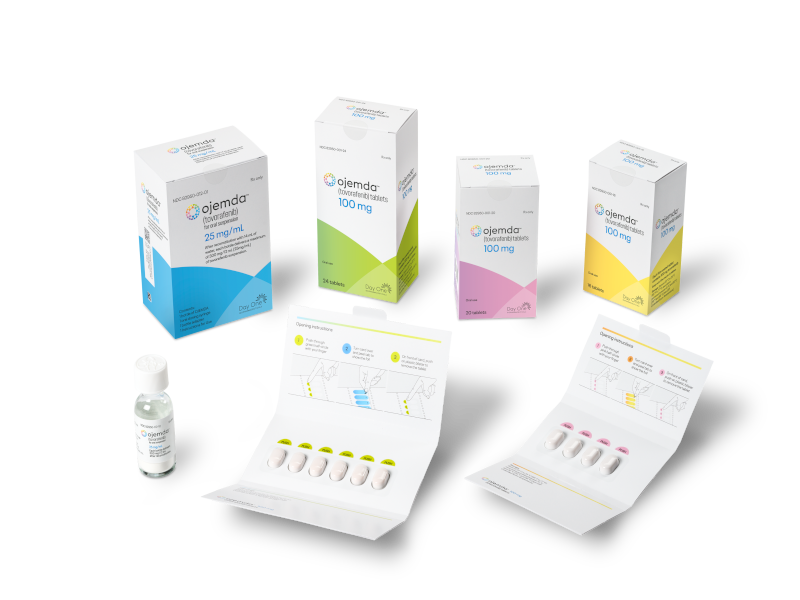
The drug is available as 100mg orange, film-coated, oval, immediate-release tablets for oral administration, as well as 25mg/ml white to off-white powder that forms a strawberry-flavoured oral suspension.
Regulatory approvals for OJEMDA
The US Food and Drug Administration (FDA) granted breakthrough therapy and rare paediatric disease designations to OJEMDA. The drug was evaluated under priority review by the FDA.
In April 2024, the FDA granted accelerated approval for OJEMDA™ based on the response rate and duration of response from the FIREFLY-1 clinical trial. Day One also received a rare paediatric disease priority review voucher from the FDA with the approval.
Tovorafenib has also been awarded orphan drug designation by the FDA for the treatment of malignant glioma and by the European Commission (EC) for the treatment of glioma.
Paediatric low-grade glioma causes and symptoms
Low-grade gliomas are the type of brain tumours that originate from glial cells, which support and nourish neurons.
pLGG is a prevalent form of brain cancer in children, often leading to severe tumour and treatment-related complications that can significantly affect the patient’s life trajectory. The BRAF gene is the most frequently altered gene in pLGG, affecting up to 75% of patients.
Children with pLGG may experience a range of symptoms, including headaches, severe vomiting, vision and balance issues, seizures, weight fluctuations, premature puberty, clumsiness, confusion, sleepiness and behavioural changes. These symptoms can often be alleviated through vomiting.
OJEMDA’s mechanism of action
Tovorafenib functions as a Type II RAF kinase inhibitor, targeting mutant BRAF V600E, wild-type BRAF, and wild-type CRAF kinases. It has demonstrated antitumour activity in cultured cells and xenograft tumour models with BRAF V600E and V600D mutations, as well as in a xenograft model with a BRAF fusion.
Clinical trials on OJEMDA
The pivotal, multi-centre, open-label, single-arm Phase II FIREFLY-1 clinical trial enrolled 137 patients with relapsed or refractory BRAF-altered pLGG across two study arms. Arm 1, which included 77 patients, was the basis for the efficacy analysis, while Arm 2 provided additional safety data from 60 patients and facilitated access to tovorafenib after Arm 1 reached full enrolment.
The primary measure of efficacy was the overall response rate (ORR), defined as the proportion of patients achieving a complete response (CR), partial response (PR), or minor response (MR) as determined by blinded independent central review (BICR) according to the Response Assessment in Paediatric Neuro-Oncology Low-Grade Glioma (RAPNO-LGG) criteria.
In Arm 1, data from 76 RAPNO LGG evaluable patients demonstrated an ORR of 51%, with 28% achieving PRs and 11% achieving MRs. Among the 64 patients with BRAF fusions or rearrangements, the ORR was 52%, and it was 50% for the 12 patients with a BRAF V600 mutation. The ORR was 49% for 45 patients who had previously received MAPK [mitogen-activated protein kinase]-targeted therapy and 55% for 31 patients who had not received a prior MAPK-targeted therapy.
The median duration of response according to RAPNO LGG criteria was 13.8 months, as of June 2023, with 66% of patients still participating in the study and continuing treatment. The median time to response after starting OJEMDA treatment was 5.3 months. Based on RANO LGG criteria, the ORR was 53%.
The most commonly reported side effects were rash, hair colour changes, tiredness, viral infection, vomiting, headache, fever, dry skin, constipation, nausea, acne and upper respiratory tract infection.
Ongoing studies
Tovorafenib is currently being evaluated as a front-line treatment for patients with pLGG in the Phase Ⅲ FIREFLY-2/LOGGIC trial. Additionally, it is being studied in combination with the MEK inhibitor pimasertib in the FIRELIGHT-1 trial, which is focused on adolescent and adult patients with recurrent or progressive solid tumours that exhibit MAPK pathway alterations.