Phesgo is a fixed-dose combination (FDC) of Perjeta and Herceptin with hyaluronidase for the treatment of human epidermal growth factor receptor 2 (HER2)-positive breast cancer and HER2-positive colorectal cancer that has progressed after chemotherapy.
The drug is eligible for use alongside chemotherapy as a neoadjuvant treatment for patients with HER2-positive, locally advanced, inflammatory, or early-stage breast cancer as part of a complete treatment regimen for early breast cancer. It is also approved as an adjuvant treatment for patients with HER2-positive early breast cancer at high risk of recurrence.
Additionally, Phesgo is suitable for use in combination with docetaxel for the treatment of patients with HER2-positive metastatic breast cancer who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease.
The formulation of Phesgo incorporates Halozyme Therapeutics’ Enhanze drug delivery technology, which facilitates subcutaneous administration.
Genentech, a member of the Roche Group and a biotech company based in the US, developed Phesgo. The strategic alliance between Chugai and Roche, established when Chugai merged with Nippon Roche in October 2002, grants Chugai exclusive rights to develop and market Roche products in Japan.
Phesgo is a clear to opalescent, colourless to slightly brownish solution for injection, available in a single-dose vial for subcutaneous administration in combination with intravenous (IV) chemotherapy.
One of the most notable advantages of Phesgo is its administration time. Phesgo can be administered over five to eight minutes, a significant reduction compared to the 60 to 150 minutes required for conventional intravenous infusion.
The shortened administration time has the potential to lessen pressure on healthcare systems by reducing the time patients spend in treatment, as well as other associated costs such as drug preparation and time spent in the infusion chair.
Regulatory approvals for Phesgo
Chugai Pharmaceutical obtained regulatory approval for Phesgo from Japan’s Ministry of Health, Labour and Welfare (MHLW) for HER2-positive breast and colorectal cancer in September 2023.
It followed the company’s initial filing of a new drug application in Japan in September 2022.
The MHLW’s decision was based on the results of the global Phase III FeDeriCa trial, in patients with HER2-positive breast cancer.
Phesgo is the world’s first subcutaneous injection for HER2-positive colorectal cancer.
The European Commission granted its approval to the drug for treating HER2-positive breast cancer in adults in December 2020.
The US Food and Drug Administration (FDA) approved Phesgo for the treatment of eligible patients with early and metastatic HER2-positive breast cancer in June 2020.
The FDA’s approval was based on the data from both the Phase III FeDeriCa and the Phase II PHranceSCa clinical trials.
HER2-positive breast cancer causes and symptoms
Breast cancer remains one of the most prevalent forms of cancer affecting women worldwide, with an estimated 15% to 20% of cases being HER2-positive.
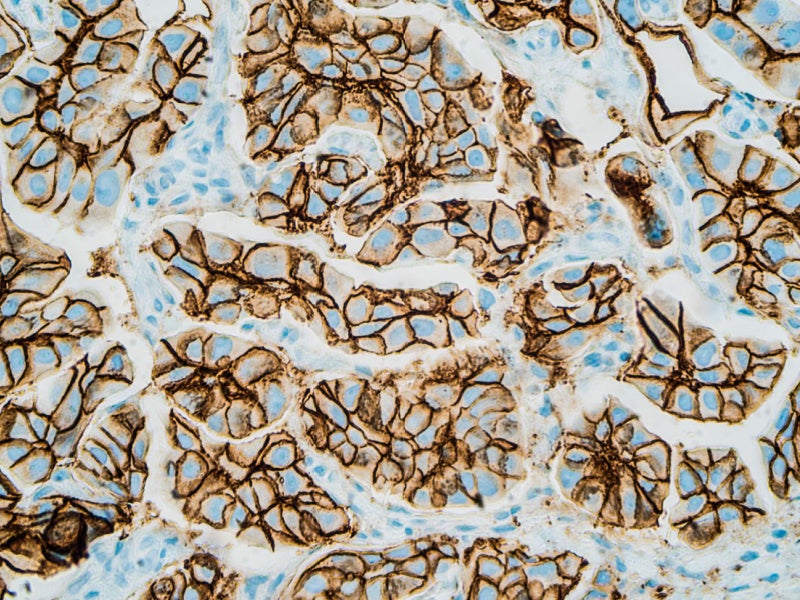
The subtype of breast cancer is distinguished by an accumulation of HER2 receptors on the surface of tumour cells, leading to accelerated growth and division compared to other cell types. The presence of these receptors is a critical factor in the formation of tumours.
HER2-positive breast cancer can be either early breast cancer, which is confined to the breast and may involve nearby lymph nodes, or metastatic breast cancer, which has spread to distant organs such as the lungs, liver, or bones.
The excess of HER2 proteins that characterise this form of cancer cannot be detected through symptoms alone. Instead, common indicators such as changes in breast shape, lumps, pain, nipple discharge, inversion, swelling, or thickening of the skin, may prompt further investigation, typically through a mammogram as part of routine screening.
A HER2 test is essential in order to confirm the diagnosis and treatment of HER2-positive breast cancer.
Phesgo’s mechanism of action
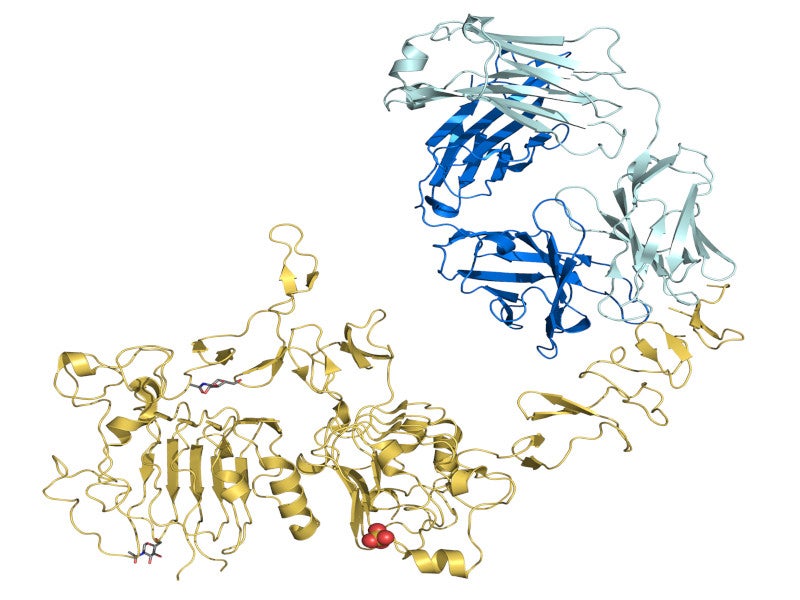
Phesgo contains the same monoclonal antibodies found in Perjeta and Herceptin, the standard therapy for HER2-positive breast cancer, in addition to vorhyaluronidase alfa, a genetic recombination.
The role of hyaluronidase, an enzyme that degrades hyaluronic acid, is to enhance the dispersion and absorption of the antibodies into the body.
The therapeutic actions of Perjeta and Herceptin are designed to be complementary. Both target the HER2 receptor but bind to distinct sites. The dual binding disrupts the signalling pathways that would otherwise promote the proliferation and survival of cancer cells.
The combination of these two antibodies in Phesgo is intended to provide a more comprehensive blockade of the HER signalling pathways, thereby inhibiting the growth of tumour cells.
Enhanze drug-delivery technology
Halozyme’s proprietary Enhanze drug-delivery technology stands out for its innovative approach to administering biologics.
The technology is based on a patented recombinant human hyaluronidase enzyme (rHuPH20), which has been instrumental in overcoming the traditional constraints associated with the subcutaneous delivery of large-volume biologics.
The rHuPH20 enzyme is a pivotal factor in Enhanze’s ability to facilitate the subcutaneous administration of biologics that were previously limited to IV routes.
Janssen’s Darzalex FASPRO, Takeda’s HYQVIA, Roche’s Herceptin, and Rituxan/MabThera are other approved products that utilise Enhanze to improve the delivery of their biologics.
Clinical trials on Phesgo
The approval of Phesgo by the FDA was based on the results from the Phase III FeDeriCa and Phase II PHranceSCa clinical trials.
The FeDeriCa trial is an international, multicentre two-arm, randomised, open-label study aimed to compare the pharmacokinetics, efficacy and safety of subcutaneous injection of Phesgo with chemotherapy against the IV infusion of Perjeta and Herceptin.
Involving 500 patients in neoadjuvant and adjuvant settings, the primary endpoint was to measure the minimum levels of Perjeta in the blood over a specific dosage interval and to assess the total pathological complete response in the breast and axilla post-surgery, indicating the absence of identifiable cancer tissue in the excised tissue.
The study sought to determine any differences between Phesgo and Perjeta + Herceptin.
The FeDeriCa study successfully met its primary endpoint of non-inferior levels of Perjeta in the blood. The geometric mean ratio for the primary endpoint was 1.22, with the lower limit of the 90% confidence interval of the GMR equal to 1.14, exceeding the pre-specified non-inferiority margin of 0.80.
It demonstrated that the levels of Perjeta in the blood were not inferior when administered via Phesgo compared to the traditional IV method.
Furthermore, a secondary endpoint concerning the non-inferior levels of Herceptin was also achieved, confirming that patients receiving the FDC of Phesgo maintained adequate blood concentrations similar to those receiving IV Herceptin.
Phesgo, when used alongside chemotherapy, exhibited a safety profile comparable to the IV administration of Perjeta plus Herceptin and chemotherapy.
The PHranceSCa study is a randomised, multicentre, multinational, open-label, crossover Phase II clinical trial aimed to evaluate patient preference and satisfaction with the SC administration of Phesgo.
The trial involved 160 patients who had completed neoadjuvant treatment with Perjeta, Herceptin, and chemotherapy, and had undergone surgery prior to randomisation.
The primary endpoint was determined by the Patient Preference Questionnaire, focusing on the percentage of participants who favoured treatment with Phesgo over the standard IV formulations of Perjeta and Herceptin.
The study found that 85% of individuals undergoing treatment for HER2-positive breast cancer favoured SC administration over IV treatment, attributed to the reduced time spent in the clinic and the more comfortable nature of treatment administration.
The most common adverse effects were hair loss, nausea, diarrhoea, anaemia (a reduction in red blood cells), and asthenia (lack of energy).
The clinical trials of Phesgo have provided substantial evidence of its non-inferiority in pharmacokinetics and efficacy when compared to traditional IV treatments.
Furthermore, the PHranceSCa study has shed light on patient preferences, indicating a potential shift towards the subcutaneous administration of cancer therapies.