Technivie (ombitasvir, paritaprevir and ritonavir) is the first direct-acting antiviral drug approved for the treatment of genotype 4 (GT4) chronic hepatitis C virus (HCV) infection in the US. The drug was discovered and developed by AbbVie.
Technivie, in combination with Ribavirin (RBV), was approved by US Food and Drug Administration (FDA) as an all-oral, interferon-free, direct-acting, antiviral treatment for adults with GT4 chronic HCV infection, who do not have cirrhosis, in July 2015.
The FDA granted breakthrough therapy designation to the drug in 2014 and approved it under priority review.
Approval marks a significant advancement as the drug provides a cure for the historically difficult-to-treat HCV population, which had limited treatment options.
Chronic hepatitis C
Chronic hepatitis C is a liver inflammation caused by the hepatitis C virus, which is a blood-borne virus that is commonly transmitted through unsafe injection practices and transfusion of unscreened blood.
There are six major types of HCV genotypes, among which GT1 is most common infection and constitutes 74% of all cases, while GT4 infection accounts for approximately 1.1% of HCV infections.
According to the Centers for Disease Control and Prevention’s (CDC) estimates, approximately 2.7 million people have chronic HCV infection in the US.
It is projected that by 2020, one million current HCV patients will develop liver cirrhosis or scarring of the liver that will result in a critical public health issue. It is also projected that HCV-related healthcare costs in the US may reach $85bn in the next 20 years.
Technivie’s mechanism of action
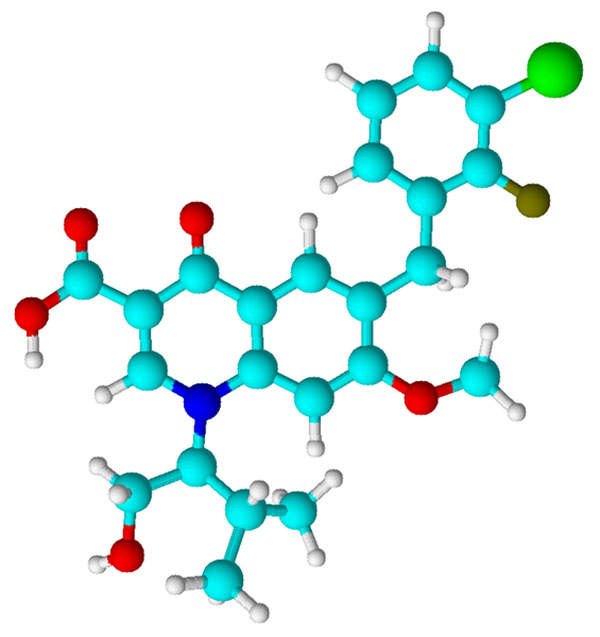
Technivie is a combination of three different ingredients, paritaprevir/ritonavir (150/100mg) and ombitasvir (25mg), in fixed doses.
Ombitasvir and paritaprevir are active and direct-acting HCV antiviral agents with distinct mechanism of action that target and inhibit specific HCV proteins in the viral replication process.
Ritonavir is an inactive agent against HCV and is a potent CYP3A inhibitor that increases peak and trough plasma drug concentrations of paritaprevir and overall drug exposure.
Dosage forms and strengths
Viekirax (ombitasvir / paritaprevir / ritonavir) and Exviera (dasabuvir) is indicated for the treatment of genotype 1 chronic hepatitis C virus (HCV) infection and compensated cirrhosis.
Technivie is available as a pink-coloured, film-coated, oblong, biconvex-shaped tablet and contains fixed doses of 12.5mg ombitasvir, 75mg paritaprevir and 50mg ritonavir. The drug is meant for oral administration only.
Clinical trials on Technivie
The FDA approval of Technivie is based on results from a Phase II clinical trial called Pearl-I, which was conducted to determine the drug’s safety and efficacy in patients affected with GT4 chronic HCV, without cirrhosis.
Results of the trial showed 100% sustained virologic response rates at 12 weeks post-treatment.
Pearl-I was a randomised, multicenter, open-label study that enrolled 135 subjects with HCV GT4 infection without cirrhosis, who were new to therapy (treatment-naive) or were unresponsive to the earlier treatment with pegylated interferon/ribavirin (PegIFN/RBV).
Treatment-naive subjects were randomised to receive one ombitasvir 25mg tablet, three paritaprevir 50mg tablets and one ritonavir 100mg capsule, with or without ribavirin, once a day with food, for 12 weeks.
Treatment-experienced (those who were earlier treated with PegIFN/RBV) patients received one ombitasvir 25mg tablet, three paritaprevir 50mg tablets and one ritonavir 100mg capsule, with ribavirin once a day, with food, for 12 weeks.
The dosage of ribavirin varied between 1,000mg and 1,200mg a day based on the weight of the subject. The primary endpoint was the sustained virologic response defined as HCV RNA below the lower limit of quantification.
Results showed that 100% subjects in treatment-naïve and treatment-experienced group that received RBV along with Technivie achieved SVR12, while 91% of treatment-naïve group that were not treated with RBV achieved SVR12, the primary endpoint of the study.
Most common adverse events recorded during the trial were asthenia (weakness), fatigue, nausea and insomnia.