VIMPAT® (lacosamide) is a federally-controlled drug (CV) indicated as a supplementary therapy for the treatment of primary generalised tonic-clonic seizures (PGTCS) in patients aged four years and older.
VIMPAT’s label has also been expanded for the treatment of paediatric patients with epilepsy for either monotherapy or supplementary therapy for the treatment of partial-onset seizures in patients aged four years or older.
It is available in three types of formulations, oral tablets, oral solution and sterile solution for injection. Oval, film-coated tablets are available in four dosage strengths, 50mg (pink-coloured), 100mg (dark yellow-coloured), 150mg (salmon-coloured) and 200mg (blue-coloured).
The oral solution is a clear, colourless to yellow or yellow-brown, strawberry-flavoured liquid in 10mg / ml dosage strength, while intravenous (IV) injection is available as clear, colourless sterile solution in single-dose vials with 200mg / 20ml dosage strength.
VIMPAT approvals
VIMPAT was initially launched in the European Union as a supplementary therapy for the treatment of partial-onset seizures with or without secondary generalisation in adult and adolescent (aged 16-18 years) epilepsy patients in August 2008.
The drug received approval from the US Food and Drug Administration (FDA) as an add-on therapy for the treatment of partial-onset seizures in adult patients with epilepsy in 2008.
Further, the FDA approved the drug as a monotherapy for the treatment of partial-onset seizures in adults with epilepsy aged 17 years and older in August 2014.
In 2017, the drug was approved as a monotherapy or adjunctive therapy in paediatric patients aged four years and older with partial-onset seizures in the US and Europe.
In October 2020, VIMPAT received a positive opinion from the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) for the treatment of PGTCS in patients with idiopathic generalised epilepsy (IGE).
VIMPAT (lacosamide) CV received the FDA approval as a supplementary therapy to treat PGTCS in November 2020.
It is currently approved in 72 countries and is under regulatory review in Japan and Australia for the treatment of PGTCS.
Primary generalised tonic-clonic seizures (PGTCS) causes and symptoms
PGTCS are seizures that occur in the entire brain, involving both cerebral hemispheres, resulting in stiffening of the muscles and convulsions that last for up to a few minutes. It is a type of manifestation of epilepsy, a chronic brain disorder affecting approximately 65 million people worldwide.
People diagnosed with PGTCS are more likely to be hospitalised and the probability of sudden unexpected death is 15 times higher in patients who experience three or more convulsions in one year.
Symptoms of PGTCS may include a strange feeling or sensation (an aura), involuntary screaming or crying, losing control of the bladder and bowels during or after the seizure, unconsciousness and waking up in the confused state and extreme headache after the seizure.
Lacosamide’s mechanism of action
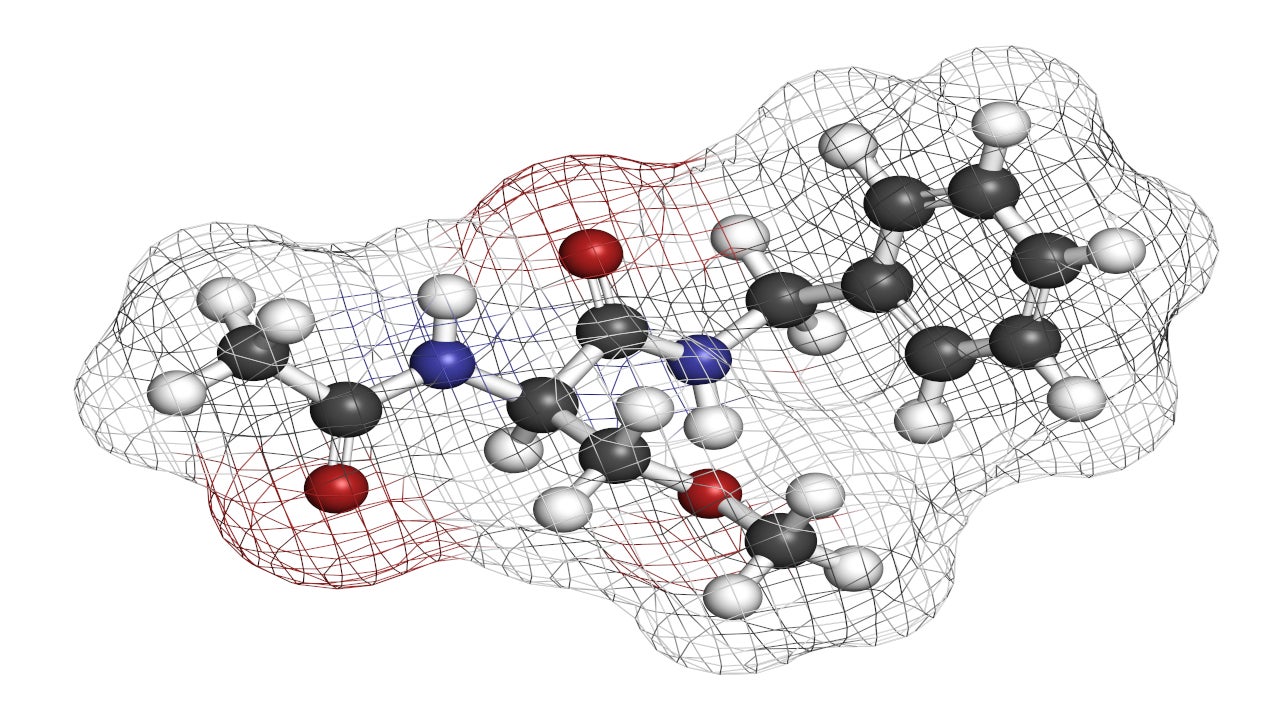
Lacosamide is a functionalised amino acid belonging to a class of anti-epileptic or anti-convulsion drugs.
It improves the gradual inactivation of sodium voltage-gated channels selectively, resulting in the stability of hyperexcitable neuronal membranes and inhibition of repeated neuronal firing.
The decreased activity of the sodium channels enables the transfer of electrical impulses between nerve cells.
Clinical trials on VIMPAT
FDA approval of VIMPAT was based on the results of phase three, randomised, double-blind, multi-centre, 24-week clinical study that enrolled 242 PGTCS patients with IGE aged four years and older, to evaluate the efficacy of the drug.
The primary endpoint of the study was the time to second PGTCS during the 24-week (166-day) treatment period.
Patients were randomised to receive a fixed-dose dosing regimen of either VIMPAT (n=121) or placebo (n=121) twice daily.
The risk of experiencing a second PGTC seizure decreased substantially by 45% in patients who received VIMPAT compared to the placebo group, over the 24-week treatment period.
Frequent adverse reactions observed in patients during the clinical trial were dizziness, drowsiness, headache, nausea and double vision.