Zactima (vandetanib) is an orally available tyrosine kinase inhibitor (TKI) developed by AstraZeneca for the treatment of solid tumours.
In July 2009, AstraZeneca submitted a new drug application to the US Food and Drug Administration (FDA) and a marketing authorisation application to the European Medicines Agency for Zactima as a treatment for non-small cell lung cancer. The application was backed by data from Phase III clinical trials.
However, in October 2009, AstraZeneca announced that it had withdrawn both filings. The decision was taken after an updated analysis of clinical data, which indicated that Zactima with chemotherapy resulted in no significant improvement in the overall survival rate of patients with non-small cell lung cancer.
The decision was also based on preliminary feedback from the regulatory authorities, who said that the clinical data presented was not sufficient for approval. AstraZeneca has now discontinued the development of Zactima for this indication.
Zactima was investigated as a treatment for thyroid cancers. It was granted orphan drug status by the FDA for the treatment of follicular, medullary, anaplastic, locally advanced and metastatic papillary thyroid cancers. In January 2010, the company announced positive results from Phase II studies in medullary thyroid cancer, a rare malignancy associated with poor prognosis and one for which there are very few treatment options.
In June 2010, AstraZeneca announced positive results from a phase III clinical trial in patients with medullary thyroid cancer. The company filed a marketing authorisation application and new drug application for this indication in September 2010.
In April 2011, AstraZeneca received approval from the FDA for zactima for the treatment of medullary thyroid cancer. Zactima is currently being reviewed in the European Union and Canada.
Tyrosine kinase inhibitors
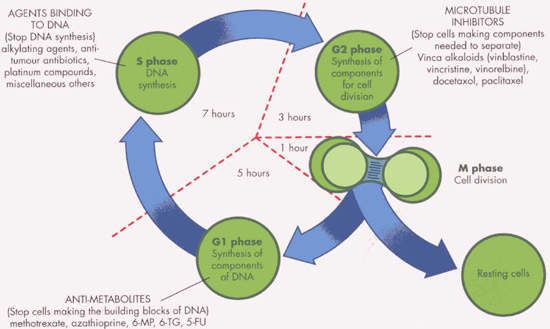
Protein tyrosine kinases are enzymes that provide a central switch mechanism in cellular signal transduction pathways. As such, they are involved in many cellular processes such as cell proliferation, metabolism, survival and apoptosis.
Several protein tyrosine kinases are known to be activated in cancer cells and to drive tumour growth and progression. Blocking tyrosine kinase activity therefore represents a rational approach to cancer therapy.
Zactima is an orally active inhibitor of vascular endothelial growth factor (VEGF) receptor-2 tyrosine kinase with additional activity against epidermal growth factor receptor (EGFR) tyrosine kinase, a property it shares with Iressa (gefitinib).
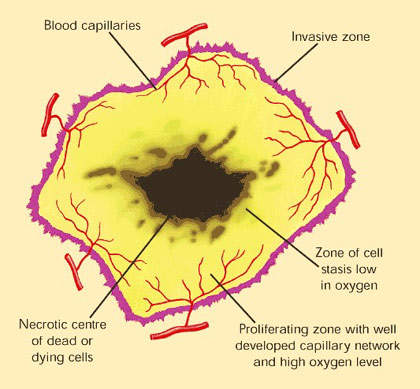
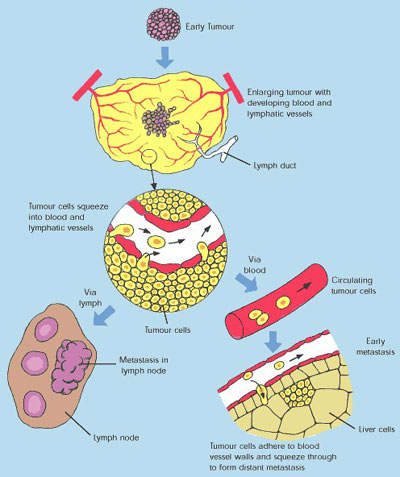
VEGF is a pro-angiogenesis factor that binds to receptors on blood vessels and stimulates the growth of new blood vessels, an important process in the spreading of tumours.
By inhibiting the action of VEGF, Zactima also acts as an angiogenesis inhibitor. Thus, Zactima exerts its anti-tumour effects by a variety of mechanisms. In this respect it differs from Iressa, which is a selective EGFR-TKI.
Zactima clinical trials
The preliminary results of the Phase II trial were presented at the American Society of Oncology annual meeting in May 2005, and showed that Zactima in combination with docetaxel increased progression-free survival. Although the combination regimen did not increase overall survival, the secondary clinical endpoint, it was suggested that this might have been due to the relatively small number of patients studied.
Phase III evaluated the safety and effectiveness of 100mg of vandetanib in combination with chemotherapy. Phase III comprised five randomised, double-blind, placebo-controlled trials: Zodiac, Zeal, Zest, Zephyr and Zeta. AstraZeneca submitted the results of the first three to the American Society of Clinical Oncology in May 2009.
Zodiac was conducted to assess the combination of 100mg of vandetanib with docetaxel versus docetaxel alone. Results from the Zodiac study demonstrated that the addition of vandetanib to docetaxel led to significant improvement in progression-free survival, the duration a patient survives without occurrence of cancer. The study recruited 1,391 patients at 250 centres across Europe, North America, South America and Asia-Pacific.
Zeal assessed the effectiveness of the combination of 100mg of vandetanib with pemetrexed against pemetrexed alone. The study did not demonstrate any significant prolongation of progression-free survival (PFS) compared with pemetrexed. The study recruited 534 patients at 160 centres in more than 23 countries.
Zest studied the efficacy of 300mg of vandetanib against 150mg of erlotinib. The study did not meet its primary objective of prolongation of progression-free survival for vandetanib. The study recruited 1,240 patients diagnosed with advanced or metastatic non-small cell lung cancer and who had undergone one failed anti-cancer therapy.
Zephyr was a randomised, double-blind, parallel-group, multi-centre study testing the effectiveness of 300mg of Zactima in combination with best supportive care against best supportive care, in patients diagnosed with locally advanced or metastatic (stage IIIB-IV) non-small cell lung cancer who had undergone therapy with an EGFR inhibitor. The study was carried out in 170 centres in more than 23 countries.
The FDA approval for Zactima was based on the ZETA (Zactima Efficacy in Thyroid Cancer Assessment) study. The double-blind and randomised study enrolled 331 patients and assessed 300mg daily dosage of zactima as a monotherapy in advanced medullary thyroid cancer compared to placebo.
The study results demonstrated that the patients who were randomised with zactima showed a significant improvement in PFS when compared to placebo-administered patients. The median PFS was 22.6 months in zactima-administered patients, whereas it was 16.4 months in placebo-administered patients. The common adverse reactions to the drug were diarrhoea, rash, acne, nausea, headache, hypertension, fatigue, decreased appetite and abdominal pain.
Improving treatment options for lung cancer patients
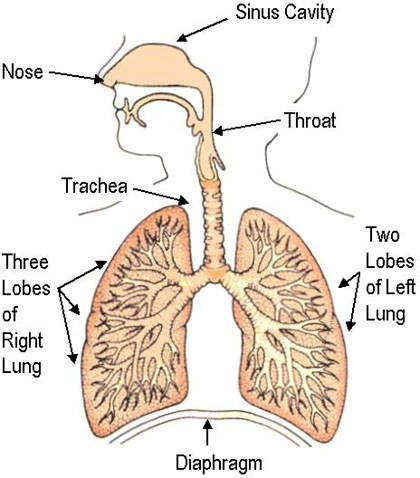
Since 1985, lung cancer has been the most common cancer in the world and it remains the major cause of all cancer-related deaths, especially among men. In 2002 lung cancer claimed 1.18 million deaths worldwide, 17.6% of the world total.
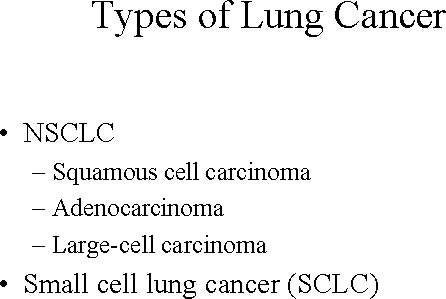
Cancers of the lung are of two types: non-small cell lung cancer and small-cell lung cancer. Non-small cell lung cancer is the most common, accounting for around 80% of all lung cancers. It is an aggressive disease, for which overall five-year survival is generally less than 10%.
Treatment of lung cancer has traditionally centred on the use of surgery, for operable cases, radiotherapy and chemotherapy with cytotoxic drugs. Platinum-based regimens are the mainstay of chemotherapy and include cisplatin and carboplatin. To enhance the efficacy of these agents, platinum-based agents may be combined with taxanes, such as paclitaxel and docetaxel.
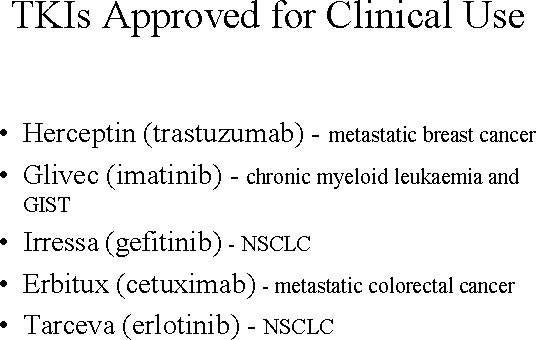
Targeted agents such as TKIs are seen as an important development with potential to improve treatment outcomes in patients with non-small cell lung cancer. Currently approved TKIs for non-small cell lung cancer include Iressa (gefitinib) and Tarceva (erlotinib).
Marketing commentary
The market for antineoplastic drugs is the third largest sector of the prescription drug market, behind cardiovascular and central nervous system drugs, and is currently experiencing strong growth. Significant opportunities exist for effective new treatments for lung cancer, which are among the most difficult cancers to treat.
Despite the disappointment with Iressa, the recent approval of Tarceva for second-line use in anti-neoplastic drugs patients failing at least one prior chemotherapy regimen suggest that TKIs have a place in the treatment of lung cancer.
Zactima is a once-daily, oral TKI that combines the action of Iressa and Tarceva with an additional ability to deprive tumours of their blood supply via VEGFR-2-mediated antiangiogenic effects. A broader spectrum of anti-tumour activity may confer treatment advantages but this awaits confirmation in large-scale trials.