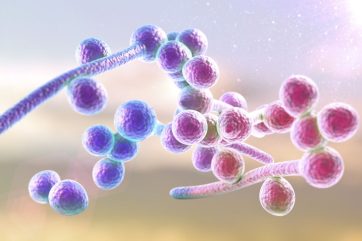
New treatments for candidiasis are of high significance as the common fungal infection can lead to immense discomfort for patients around the world. Caused by the yeast candida, candidiasis can even have serious consequences for those with compromised immune systems.
According to GlobalData, since January 2022, 145 clinical trials investigating the disease have been conducted, with a further 46 planned and 19 currently in progress. These trials are becoming ever more important as drug-resistant strains of the disease continue to emerge.
There are many different variations of candidiasis, whose pervasiveness varies according to different geographic and demographic factors. Candida albicans is the most common variant overall, while regionally variations in C glabrata, C tropicalis, and C parapsilosis can be more prevalent. When non-invasive, and affecting only mucosal surfaces or superficial skin layers, the disease can be treated with topical over-the-counter treatments or prescriptive azoles, including suppositories.
Invasive candidiasis, on the other hand, can have serious, life-threatening consequences. The fungus can spread to attack the eyes, heart, and kidneys, and requires careful primary treatments, typically intravenous echinocandins supplemented by fluconazole or amphotericin B. However, such treatment can become complex due to drug-resistant strains of the disease, the limited tissue penetration of some antifungals, and the potential toxicity of drug interactions. For patients to have the most successful recovery possible, a better understanding of candidiasis is required, and further innovative treatments must be trialled.
Factors affecting the spread of candidiasis
Invasive candidiasis is widespread in South and Central America in areas with limited healthcare resources and inadequate infection controls. Elsewhere in the world, the rate of infection varies. In Asia, Thailand reports a high number of cases compared to Malaysia. In Europe, there is a greater frequency of cases in Hungary versus Germany, Belgium, and Portugal.
Susceptibility to invasive candidiasis appears to vary by demographic. Black and African American individuals in the US are disproportionately affected by the fungal infection alongside the elderly and immunocompromised. To understand these discrepancies, more research must be done, especially with the increased prevalence of non-albicans candida spp., azole resistance, and the emergence of candida auris.
Funding for innovative candidiasis treatments
According to a recent report titled Candidiasis – Global Clinical Trial Landscape by leading contract research organisation (CRO) Novotech, over the past six years the global biotech and biopharmaceutical industry has launched more than 200 clinical trials investigating candidiasis.
The Asia-Pacific region dominates, conducting over 60% of trials, which are predominantly taking place in China. Most of these are Phase I trials, indicating a focus on early exploration. Elsewhere, countries with well-developed pharmaceutical markets such as the US, Germany, and Belgium are making significant contributions, with a greater range of trials across Phases I, II, and III. However, the Asia-Pacific region demonstrates a compound annual growth rate (CAGR) of over 20%, outpacing Europe and North America. These numbers highlight that area’s growing significance in the advancement of medical research and patient care.
In terms of funding, public institutions such as the US National Institutes of Health (NIH) and the Biomedical Advanced Research and Development Authority (BARDA) lead candidiasis research and antifungal development. In the world of venture capital, the US and China are the most common regions for investment. The shared commitment to tackling candidiasis is evident in the rising number of Series B and C rounds, with an emphasis on the preclinical stages to develop new groundbreaking treatments.
The latest breakthroughs in antifungal medications bode well for the future of candidiasis treatment. Vaginal candidiasis was the focus of two recent projects, Brexafemme’s 2021 approval and Vivjoa, introduced in 2022 to address recurrent vulvovaginal candidiasis. Additionally, a milestone new treatment for invasive candidiasis was released in 2023 by Rezzayo.
While these tailored therapies address different patient needs, the quest for a licensed antifungal vaccine continues. Clinical trials are continuing this work through a variety of strategies, including small molecules such as Cresemba that currently lead Phase III trials. As vaccine development continues and new treatments emerge, the world will benefit from enhanced protection against candidiasis and innovative new methods of treating it.


